The Great Blood Pressure Scam
Wed 3:45 pm +00:00, 31 Jul 2024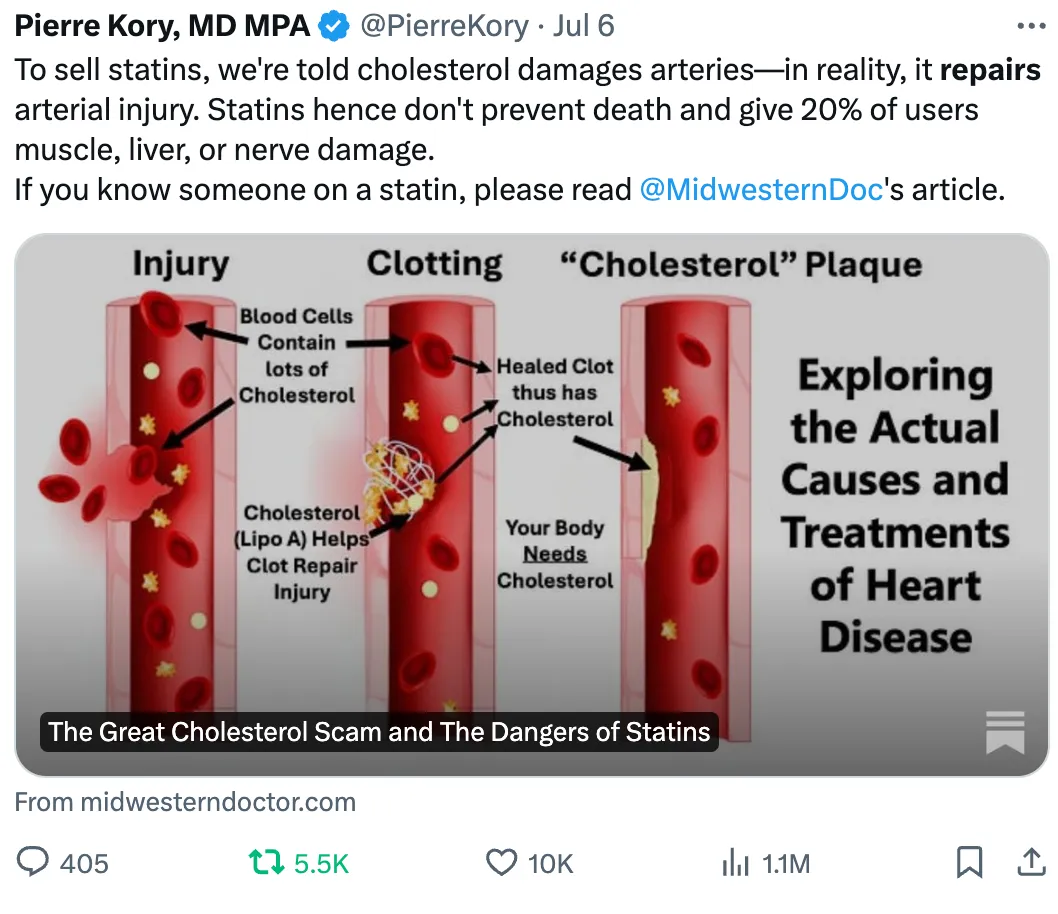
Exploring the Forgotten Causes and Treatments of Hypertension and the Dangers of BP Medications
Story at a Glance:
•Elevated blood pressure is the most common chronic disease, and as the decades go by more and more people are declared hypertensive.
•Remarkably, at least 25% of all hypertension diagnoses are due to inaccurate measurements, and there is still no known reason for why over 90% of people are hypertensive.
•Aggressively treating everyone’s blood pressure is justified under the belief it prevents cardiovascular disease. However, in most cases it has never been proven to reduce heart disease—rather it only leads to a small reduction in strokes (hence why these medications were rebranded to treat “cardiovascular disease”).
•Many of the misunderstandings with heart disease arise from the fact that impaired circulation or damage to the blood vessels will cause blood pressure to go up and their correlation being misinterpreted to instead believe high blood pressure causes cardiovascular disease.
•In this article, we will discuss the actual causes of high blood pressure, the dangers of commonly used blood pressure medications, the safest pharmaceutical and natural ways to reduce blood pressure directly, and our preferred methods for treating the underlying causes of high blood pressure.
Ever since I first encountered the medical field, something struck me as off about their relentless focus on blood pressure. Before long, I began to notice that the blood pressures the same acquaintances (e.g., relatives or friends) shared with me varied immensely. As I was pondering this, a long-time Eastern spiritual teacher shared with me their belief that the West’s relentless focus on blood pressure was due to it being much easier to measure than blood perfusion (healthy blood flow).
Then, as I became more acquainted with the medical field, I began to notice a consistent pattern—whenever a drug existed that could treat a number or statistic, as the years went by, the acceptable number kept on being narrowed, making more and more people eligible to take the drugs that treated the number.
For example, as I discussed recently, once the statins drugs entered the market (which unlike their predecessors, could effectively lower cholesterol), the acceptable blood cholesterol levels kept on being lowered, and before long almost everyone was told they would die from a heart attack unless they started a statin—despite statins have an almost non-existing mortality benefit (e.g., taking them for 5 years at best makes you live 3-4 days longer) and causing (often severe) side effects for roughly 20% of users. Broadly recommending these drugs hence appears unconscionable, but as I showed in that article, these unjustifiable guidelines were a product of clever pharmaceutical marketing and targeted bribery of public officials.
In this article, I will attempt to show how something similar happened in the field of blood pressure. As this is an immensely controversial position to take (e.g., measuring and documenting blood pressure is one of the most routine procedures during a medical visit), I’ve done my best to clearly present the evidence for this perspective so you can make your own determination.
Conventional Blood Pressure Perspectives
Since blood vessels are elastic structures filled with fluid, that fluid holds them under pressure. Blood pressure in turn is typically measured by determining how much external force is needed to exceed the artery’s pressure and compress it so that blood no longer flows through it. Low blood pressure (hypotension) is a problem because it prevents blood from reaching the areas where it’s needed (e.g., orthostatic hypotension or POTS describes a common condition where people become lightheaded as they stand up due to insufficient blood being pushed into the brain), but in most cases, medicine instead focuses on the consequences of high blood pressure. Within the existing model, those consequences are:
•Weakened blood vessels become more likely to break open and leak as higher blood pressure pushes against them. This for instance is why Emergency Rooms aggressively lower the blood pressure of patients who show up with symptoms of “hypertensive emergency” such as a severe headache and a significantly elevated blood pressure. Likewise, whenever a critical blood vessel ruptures (e.g., the aorta or one in the brain), once the bleed has been confirmed, the first step in managing it is to lower the patient’s blood pressure (so less blood leaks out) after which they are sent to surgery.
•Excessive pressure on the arteries strains and damages them, causing the lining of the vessels to become damaged and gradually develop atherosclerosis.
•Excessive blood pressure damages the internal organs (termed end-organ damage), leading to premature failure and early death (e.g., from a heart attack or kidney failure).
Because of this, high blood pressure is viewed as one of the greatest preventable causes of cardiovascular disease and thus a chief focus of all medical visits is ensuring a patient achieves a sufficiently lowered blood pressure.
Unfortunately, that chain of logic has quite a few gaps in it (see if any jump out to you). We will now examine each of them.
Variable Blood Pressure
Blood pressure (BP) is immensely variable. For example, pressures at the periphery (where BP is typically measured), which when studied is found to vary by around 14 points This thus frequently leads to individuals being erroneously diagnosed with hypertension and put on blood pressure lowering medications despite having normal blood pressures (leading to those medications making them hypotensive).
This phenomenon in fact is so common (constituting 15-30% of hypertension diagnoses) that it is often referred to as “White Coat Hypertension,” a name derived from the fact stress is one of the things which commonly elevates blood pressure, and since visiting a doctor is a stressful experience, many patients hence have temporarily elevated blood pressures there. Because of this, the guidelines suggest having patients who are diagnosed with hypertension have multiple measurements to confirm it (e.g., with home blood pressure monitoring). Unfortunately, this often does not happen in practice.
Note: one common source of error when measuring blood pressure is the wrong sized cuff being used for the patient. Another is that patients frequently have significantly different blood pressures in each arm. This helps to explain why it is commonly estimated that 25% of those diagnosed with hypertension do not have it.
Likewise, there is a surprisingly poor correlation between peripheral blood pressure and the central blood pressure inside the aorta. For example, one large study found a significant difference between the blood pressure within the aorta and the arm, and that the aorta pressure had a much stronger correlation to the likelihood of cardiovascular disease.
Note: different classes of blood pressure medications have very different effects on central versus peripheral blood pressure.
What Affects Blood Pressure?
If fluid at a set pressure tries to move through a tube, as the tube shrinks, the pressure it creates (e.g., on the walls of the tube) will increase, while if the tube enlarges, the pressure it exerts will decrease. The body in turn continually controls where blood in the body goes by changing the heart rate and fully or partially constricting the arteries, allowing it to shunt blood to where it is most needed (e.g., by dilating arteries in that area).
Blood pressure is thus a product of two factors: the amount of blood in the arteries and the constriction or relaxation of the arteries containing it.
Note: since arterial BP is greater than venous BP, it’s what’s measured externally (as veins compress long before arteries do and only arterial blood has a signature pulsatile wave created by the heartbeat).
Since each beat of the heart pushes blood into the arteries and hence increases the pressure within them, two different blood pressure values exist—the baseline pressure (known as the diastolic pressure) and the pressure when the heart contracts (known as systolic pressure). The blood pressure values you see (e.g., 140/90), represent that maximum and minimum.
Note: one reason why this stretching is important is because when the vessels contract back to their normal size once the systolic pressure fades, that recoil pushes blood further along into the circulation.
Blood pressures lowering medications in turn work by loosening the arterial walls, reducing the total blood in circulation, weakening the contraction of the heart, or a combination of all three.
What Causes High Blood Pressure?
Most cases of high blood pressure (90-95% of them) are what is known as “essential hypertension” or “primary hypertension” which is a fancy (and rarely questioned) way of saying “elevated blood pressure without a known cause.” More importantly, the fact there is no known cause for most cases of elevated blood pressure has been a widespread belief in medicine for decades. Typically, the only cause we hear about is “eating salt,” despite the fact that the most detailed review of this subject found that drastic salt reduction typically results in less than a 1% reduction in blood pressure.
For the remaining 5-10% (known as secondary hypertension), recognized causes include reduced blood flow to the kidneys (which sets off a signal to raise the blood pressure because the kidney believes there isn’t enough blood perfusion), sleep apnea, or having a rare tumor which dumps large amounts of adrenaline into the blood (which constricts blood vessels and increases the heart rate).
Note: a kidney (especially the left) being in the wrong position (which is quite common) can functionally compress the renal artery. However, until an actual stenosis (narrowing) of the artery, this can be quite difficult to identify with conventional measurements. Additionally, as I showed in a recent article on the importance of sleep, poor sleep is immensely damaging to cardiovascular health and those effects extended to blood pressure (e.g., one study found a single night of partial sleep deprivation raised SBP [systolic blood pressure] by 6, another found SBP raised by 6 and DBP by 3 while a third study found it raised SBP 4.5 and DBP by 2.6 alongside using fMRI imaging to show it also impaired the brain’s control of blood vessel function).
Since the cause of hypertension isn’t known, medicine thus focuses on specific risk factors that are known to be associated with it such as being over 65, having diabetes, eating too much salt, insomnia, obesity, not exercising, stress, being an alcoholic or other people in your family having high blood pressure. Keep these risk factors in mind as you read the next section.
Note: of these causes, I and many of my colleagues believe one of the most underappreciated ones is anxiety, as frequently, effectively treating it can resolve a case of high blood pressure, which would otherwise receive (often indefinite) pharmacologic treatment.
Inverted Causality
Frequently, when you dig into medical myths, you discover that many of the dogmas myths that underlie a popular drug are actually sales slogans a marketing company created. For instance, Dr. Kory and RFK Jr. recently shared my article about statins, which went viral on Twitter because so many have been harmed by that marketing myth.
Likewise, I’ve previously discussed how:
•A chemical imbalance from low serotonin was never linked to depression (in fact patients who commit suicide are found to have elevated brain serotonin).
•Acid reflux is due to too little acid in the stomach (as acidity gives the stomach’s opening the signal to close). However, in medical school, we are always taught it is due to too much acidity.
•”Sleeping” pills are actually sedatives that block the restorative phase of the sleep cycle.
Each of these drugs in turn is immensely harmful to their users, but due to how effectively these myths were established (just like “safe and effective”) they continued to be used by large numbers of people and harm them.
I long wondered something similar about blood pressure. Does rising blood pressure damage arteries, or does damage to the circulation raise blood pressure? For example, significant plaque within the artery that feeds the kidney raises blood pressure, so why does that have to be an isolated example?
For instance, once the outflow from the heart gets obstructed (e.g., through aortic stenosis) the heart’s left ventricle is known to become enlarged (LVH), yet we typically ascribe the hypertension associated with LVH to being the cause of it rather than a result of it. Similarly, if the blood flow through the lungs gets obstructed (due to pulmonary hypertension), the right heart ventricle enlarges (RVH) and eventually fails. In certain cases, this hypertension can be immediately reversed (e.g., if it’s being caused by chronic blood clots entering the lungs), at which the heart immediately recovers, much in the same way the blood pressure immediately drops if the kidney’s blood flow is restored.
Atherosclerosis and Blood Pressure
Many of us initially became suspicious of the existing blood pressure paradigm because we noticed that circulatory impairments would proceed or occur in tandem with elevating blood pressures (rather than happening long after an elevated blood pressure had had time to damage the arteries). Because of this, each person I asked came to a similar conclusion—the increased blood pressure must be a compensatory mechanism the body is using to counteract the fact it can’t get enough blood to where it is needed (which again is recognized to occur with the kidney).
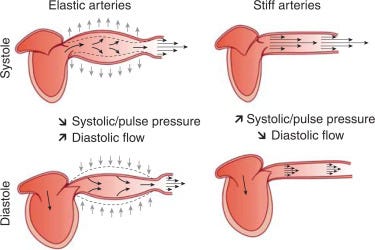
As I looked further into this, I found a few ways to explain how this could be happening. First, if you consider the earlier illustration of the circulatory cycle:
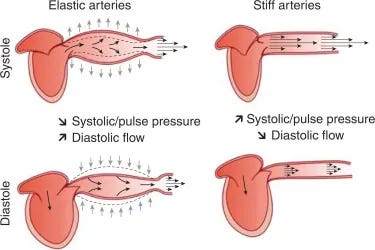
It should be clear why calcification of the arteries (which stiffens them) also increases blood pressure, as they can no longer expand as effectively and release the pressure within them.
However, there are also three other reasons why this could occur.
First, measuring blood pressure utilizes an external cuff to pressurize the arteries until the blood flow cuts off. If the artery has stiffened, however, that is much harder to do. Because of this, when patients have severe atherosclerosis, their blood pressure is no longer measured in the arm’s arteries (as the arteries there won’t compress from the cuff). At the same time, however, there is most likely a gradual stiffening that leads to the measured blood pressure being higher than it actually is.
Second, the health of the cardiovascular system to a large extent depends upon the lining of the blood vessels being able to secrete nitric oxide, which in turn dilates the blood vessels, locally decreasing blood pressure and regionally increasing blood flow. This dysfunction typically precedes the development of atherosclerotic plaques and is much more severe by the time they’ve formed (as the surface of the endothelium has calcified at that point). Because of this, many believe the core issue is not calcification of the arteries or high blood pressure but rather endothelial dysfunction (which in turn leads to abnormal growth of the endothelium and harmful blood clots forming). Given that endothelial dysfunction happens to increase blood pressure, that again argues that the direction of causality for heart disease is incorrect.
Third, whenever the body is not getting enough blood, a sympathetic reflex will be triggered to increase the blood pressure (e.g., the heart rate rises and blood vessels tighten). For example, this is commonly seen in critically ill patients or those who have rapidly lost a significant amount of blood, at which point the blood vessels will tighten and the heart rate will increase.
Zeta Potential and Blood Pressure
My original goal with this publication was to bring awareness to zeta potential as it was an almost completely unknown concept, immensely important for human health and vitality (e.g., it underlies many COVID vaccine injuries), which explained the benefits behind many renowned holistic therapies, and unlike many of the other forgotten sides of medicine, was very easy to treat.
Typically when substances are mixed in water (e.g., most biological systems), they form colloidal suspensions where the particles are kept from clumping together and instead become suspended throughout the liquid. As there are always forces (e.g., gravity or molecular attractions) that push the suspended particles together, colloidal stability is thus a property of if there are enough repulsive forces to keep them separated.
Zeta potential qualifies the electrical charge difference between each colloidal particle and its surroundings. Most living systems in turn rely upon their particles having a sufficiently negative zeta potential to repel the particles they are surrounded by. Because of this, if the net charge of a colloidal system is made more negative, the particles will become more dispersed, while if it becomes more positive, they will begin to clump together, forming successively larger colloidal agglomerations.
As the body depends upon the continual circulation of fluids, this clumping can be extremely problematic. For example, once red blood cells clump together, microstrokes often follow. As vaccines are highly effective agents at destroying the negatively charged physiologic zeta potential (particularly due to the aluminum and now spike proteins they contain—each of which carries a very strong positive charge), a wide variety of side effects result from vaccination, the most frequent of which are neurological issues (due to the brain being immensely sensitive to microstrokes)—which with basic neurologic training can be easily recognized.
Since these circulatory obstructions can be recognized with a judicious physical examination, many have recognized the significance of this condition in the past. For instance, one of the foundational diagnoses in Chinese medicine is “blood stasis,” and many Chinese medicine practitioners have argued that blood stasis is one of the primary causes of illness.
Note: while Chinese medicine has existed for thousands of years, the emphasis on blood stasis is a relatively new occurrence, which interestingly began around the same time the smallpox vaccine entered China—an extremely harmful vaccination, with many of the injuries it caused mirroring effects Chinese Medicine attributes to blood stasis.
Blood Sludging
Likewise, approximately a century ago, many Western researchers began concluding that blood cells clumping together was a root cause of many illnesses, particularly those where a focal issue created a systemic problem (e.g., burns or cancers). This condition came to be known as “blood sludging” and was quite influential at the time, especially once it became possible to directly observe blood sludging within the body (e.g., by with the appropriate microscope looking at the blood vessels in the eyes), leading to a few discoveries (e.g., the ESR test) which are still used today. Sadly, the concept of blood sludging has largely become a Forgotten Side of Medicine and only persists today through live blood cell analysis (which is widely disparaged by conventional medicine and significantly more prone to error than the original method blood sludging researchers performed by looking into the eyes).
When I first learned of this concept, one of my immediate questions was if it underlies high blood pressure as once blood were to sludge together it would:
•Create a backlog in the circulation which would increase the pressure on it (since rather than being pushed forward, blood would instead push against the arterial walls).
•Signal the body to increase its blood pressure so the pockets of sludged blood could be pushed along.
•Directly stretch the smaller blood vessels, thereby increasing their pressure (and simultaneously “stiffen” the arteries because the clumps of sludge would have significantly more resistance to compression than dispersed blood cells).
From digging into it, I learned:
The original pioneers of blood sludging had repeatedly observed small arteries (e.g., those in the eyes) would become stretched by larger sludges.
Additionally, they observed that once the pockets of sludge formed, the pressure build-up caused plasma (the non-cellular component of the blood) to begin leaking out into the tissues (leading to things like edema), and the remaining blood thus became even more concentrated with these sludge pockets.
Note: once the zeta potential concept was applied to this phenomenon, it was noted that like other colloids, if their motion was slowed, blood cells would clump together and existing clumps would enlarge. This may in part explain why immobility and a lack of exercise are so detrimental to cardiovascular health.
The primary authors in this field also cited three papers that showed the relationship between blood sludging and blood pressure, however, I was not able to locate them and hence assess what they showed (but if you can, I’ve provided the citations here). Thus far, I’ve only been able to locate a 1949 paper on the topic, which found that out of 100 individuals with a SBP above 150, 50% had Grade 1 clumping, 45% Grade 2, 4% Grade 3, and 1% Grade 4 clumping, whereas of the 50 normal adult control subjects, only, one (2%) had Grade 1 clumping.
.Finally, to illustrate how interrelated these concepts are, since blood sludging disproportionately affected the smaller vessels (since it took significantly smaller sludges to obstruct them), the primary effect of blood sludging would be injuries akin to microstrokes. However, the larger blood vessels have their own small blood vessels (known as the vasa vasorum) which sustain the arteries. Because of this, blood sludging was frequently observed to obstruct the vasa vasorum in an identical manner to what happened in other smaller sludged vessels.
As this forgotten paper clearly shows, researchers were able to show that once the blood supply in a vessel’s vasa vasorum was impaired, it would cause the endothelial lining of the blood vessel to rapidly die and fall off, with the total damage being proportion to how much the blood supply was interrupted and how long that interruption persisted. Once this happens, those lost cells can no longer release the critical nitric oxide, clots frequently form, and the blood vessel is no longer protected from damage (as the endothelial cells create the primary protective layer of the blood vessels). Because of this, poor zeta potential is arguably a primary cause of arterial damage (and the inability of vessels to then repair themselves) and the lethal clots damaged endothelium can form.
Note: this paper led me to suspect that a significant degree of the vascular damage caused by the spike protein was actually due to it causing microclotting within the vasa vasorum.
Additionally, masses of clumped blood cells have also been directly observed to plug some or all of the capillaries of kidney glomeruli—which in turn are next to the cells that release renin (the hormone the kidneys use to raise blood pressure when there is not enough blood to the kidneys). Likewise, arterial stiffening is linked to kidney dysfunction, again showing how each of these factors is interrelated. Furthermore, the kidney is the primary organ responsible for maintaining the physiologic zeta potential (and consequently why its decline parallels the decline in zeta potential seen with old age, something we consider to be a primary cause of aging)—again illustrating how interconnected these factors are (e.g., blood pressure increases with age).
Zeta Potential and High Blood Pressure
Thomas Riddick (the engineer who pioneered the zeta potential concept) strongly believed that poor zeta potential increased blood pressure and likewise led to atherosclerosis:
From the standpoint of physical chemistry, one should differentiate between the ”first” stage of cardiovascular disease involving soft blood sludge, and what I term the “second” stage, involving rigid clots or thrombi. While the quantity and/or “degree” of soft sludge can range from sparse to heavy, it should be realized that each mobile agglomerate must be broken down into smaller sized particles as it flows along the arterial tree. The blood cells must eventually become completely discrete if they are to pass through the capillaries, whose small diameter permits the cells to pass only in single file. Considerable energy must be required to continuously break down these clumps ahead of each capillary – and then reform them past the capillary. Small wonder the workload of the myocardium is increased and blood pressure raised. Indeed, it would seem that the rise in blood pressure would be greater than is actually encountered.
Likewise, each of the doctors I know who specialized in treating zeta potential found that treating it often significantly improved blood pressure (to the point it was often one of their primary approaches).
Note: consuming more potassium and less sodium is a standard recommendation for treating blood pressure. Interestingly, this is also one component of Riddick’s zeta potential regimen.
Additionally, one of the simplest ways to partially restore zeta potential, Earthing (putting your body in direct contact with the Earth’s electrical charge such as by walking barefoot in nature), in a small study of 10 patients was found to decrease SBP by 8.6% to 22.7% (averaging at 14.3%).
Another approach for improving the physiologic zeta potential Ultraviolet Blood Irradiation (which also significantly increases blood circulation and blood perfusion throughout the body—including within arteries that have significant obstructions) has been shown to improve blood pressure. For example, as detailed in a recent article on that therapy, in one study, 12 patients with chronic kidney disease had their average SBP dropped from 180 to 145 (while their DBP dropped from 118 to 88) from laser irradiation of their blood, while another study of 34 patients with severe hypertension (not responding to medications) had a 30% reduction of both their SBP and DBP alongside a prolonged disappearance of many of their more severe symptoms (e.g., headaches dizziness and chest pains).
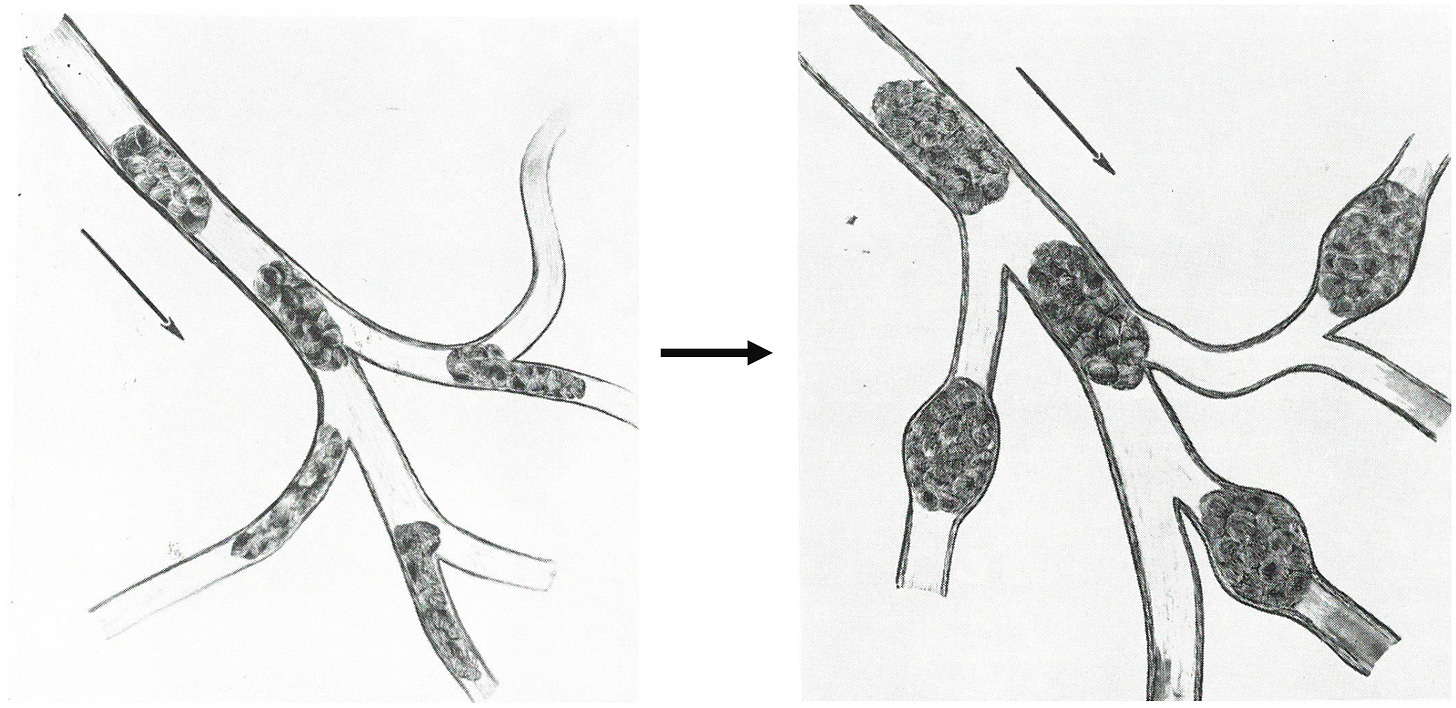
Finally, a 2019 study compared the zeta potential of 64 patients with hypertension to 50 controls. It found the controls had an average zeta potential of -23.39 mV, while hypertensive patients had a zeta potential of -16.06 mV, and that heart attack (MI) patients had even worse zeta potentials.
Note: -10mv to -15mv is the threshold where blood cells typically begin to agglomerate, while -16 to -30mv is what Riddick termed “delicate dispersion,” where they can rapidly clot when needed to (e.g., due to an arterial injury).
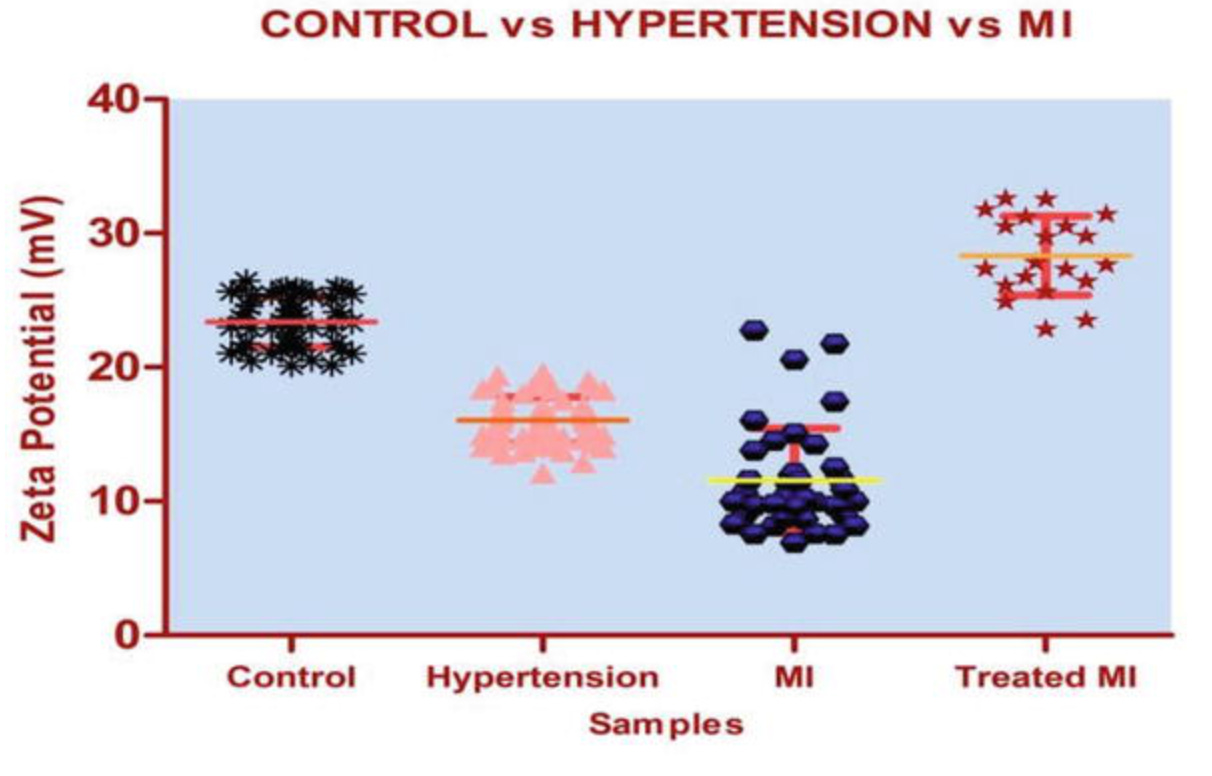
Likewise, when their blood was looked at, there was significantly greater clumping, blood cell deformation, and membrane fragility in cells from patients with cardiovascular disease:
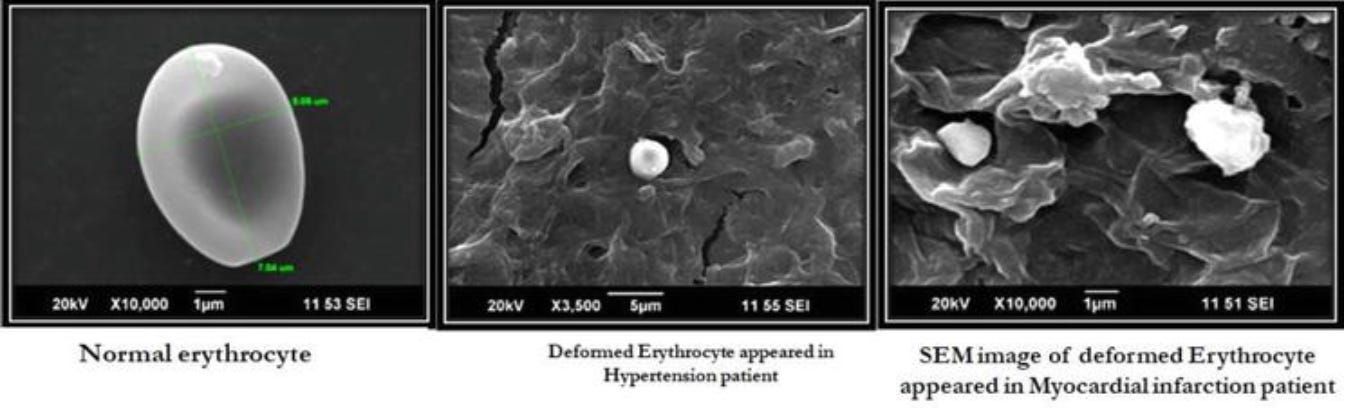
Note: Riddick (and those who followed him) frequently treated a variety of heart conditions by restoring the physiolgic zeta potential. Likewise, many holistic therapists have determined that deformed red blood cells correlate with poor health.
Hypertension and Chinese Medicine
A variety of different schools of thought exist within Chinese medicine. In those that place a higher emphasis on blood stasis, they frequently associate the condition with hypertension. For example, the acupuncturist I know who has the most experience in this area (and frequently discusses it with experts in the field) finds two common patterns in high blood pressure.
One he characterizes by the same process described by the blood sludging researchers where blood stasis will lead to extravasation (fluid leaking out of the vessels) which in turn inflames the area. This is often seen in diabetics with high blood sugar (which also impairs zeta potential), the pulse in the wrist feel stagnated, and in their school of thought, blood pressure then raises because the brain and kidneys are triggering a reflexive response to ensure they have enough perfusion.
This pattern is treatable (which includes Chinese herbs, normalizing blood sugar, losing weight and getting exercise), but takes a while to treat (as the body needs time to return to its normal homeostasis), so it’s rare to be able to find a magic bullet like a specific herb that immediately normalizes the blood pressure on its own.
In the second pattern, there is a more active, strong and full quality to the pulses (palpating them is a common way Chinese Medicine assess the body) which they believe is due to the heart or kidney not getting enough blood (due to narrowed arteries) and the heart then pumping harder to overcome that obstruction. My colleague finds this pattern is the most common in Africa American men and matches a diagnosis that used to exist within conventional cardiology (the “Water Hammer Pulse”).
Note: I suspect the predisposition he finds African American men have relates to their genetic susceptibility for salt to raise their blood pressure (something not typically observed from salt consumption).
Because of all this, he feels that using hypertensive medicines is often a bad idea since it directly opposes the body’s compensatory mechanisms for blood flow, and argues this is why hypertensive patients often require multiple medications with different mechanisms of action.
The other acupuncturist I spoke to shared that correctly targeted releases of blood stasis (which is done by bleeding specific points in the body) can be very helpful for hypertension and that he frequently sees dramatic results for hypertension with this approach.
Does High Blood Pressure Cause Heart Disease?
Note: much of the research for this section was sourced from Dr. Malcolm Kendrick.
Since high blood pressure has been observed to occur in association with heart disease and significant vascular issues such as severe headaches, strokes and organ damage can occur when blood pressure is significantly elevated (e.g., a SBP above 200), which then improves once the blood pressure is rapidly lowered, that led many to suspect high blood pressure might be the cause of heart disease—especially since blood vessel damage never occurs in low-pressure areas of the body (but do occur when blood vessels are suddenly transitioned to much higher pressures than normal such as a vein being grafted onto the heart or the blood pressure suddenly being greatly elevated in the lungs).
Unfortunately, there’s actually very little evidence that smaller elevations in blood pressure create issues. Much of the current dogma on this issue is based on a longstanding study (the Framingham study) that “found” a linear relationship between blood pressure and the risk of death—meaning that continually lowering blood pressure decreases one’s risk of dying.
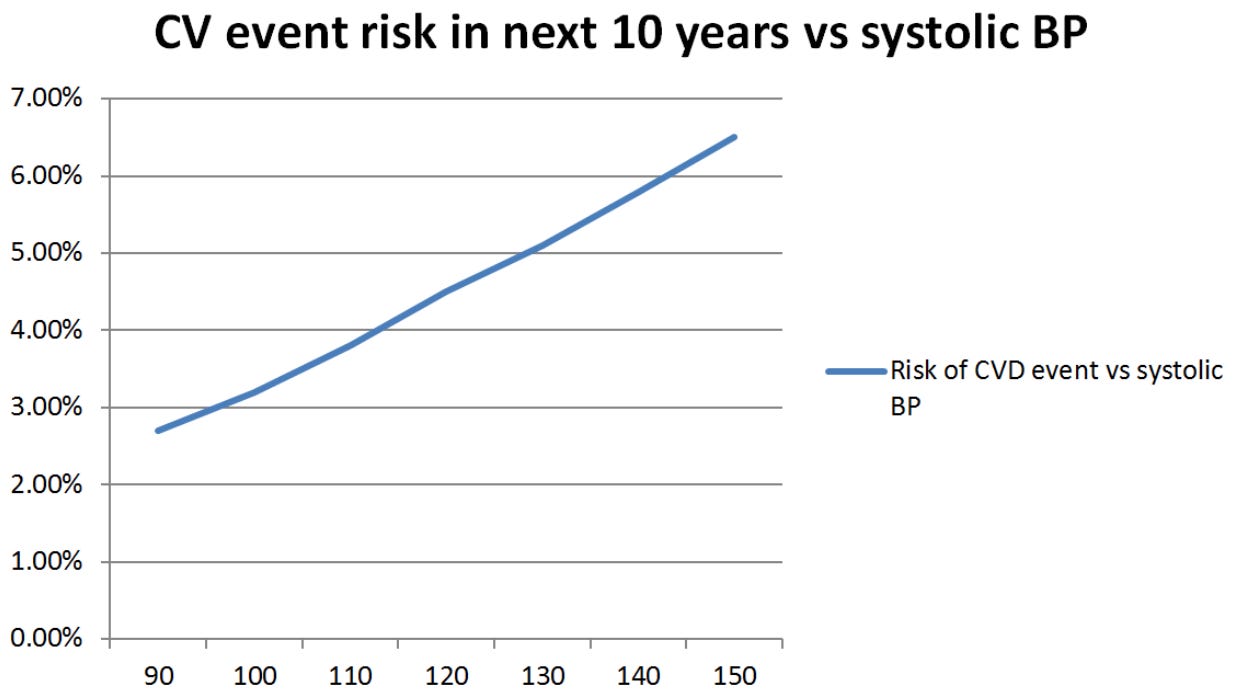
That has been the basis for many things like continual recommendations for lower and lower blood pressures or the highly erroneous cardiovascular disease risk calculator everyone uses to justify prescriptions (but was found to overestimate one’s risk of dying by 600%). This for example are the values that calculator provides for an otherwise healthy male when only their blood pressure is adjusted.
In turn, there are a few major issues with this paradigm:
•It creates a situation where no optimal blood pressure can exist, as its well known (and admitted by the NIH) that a SBP below 90 is dangerous and unhealthy.
•It’s exceedingly rare that things in biology follow a completely linear relationship.
•No one has ever done a study demonstrating that lowering blood pressure from 100 to 90 provides a benefit. Rather benefit is assumed from the linear model’s prediction.
•It was based on a flawed analysis of the Framingham study. When that data was re-analyzed in 2000, a relationship instead was found that was much more congruent with what’s typically seen in nature. Specifically, rather than being a linear relationship, blood pressure had relatively little impact on mortality until a critical threshold was passed (going above 70-80% of the normal blood pressure for the person’s age and gender), and which point there was an exponential rise in their risk of death. For example, this was a comparison between these two models for patients between 56-64 years of age:
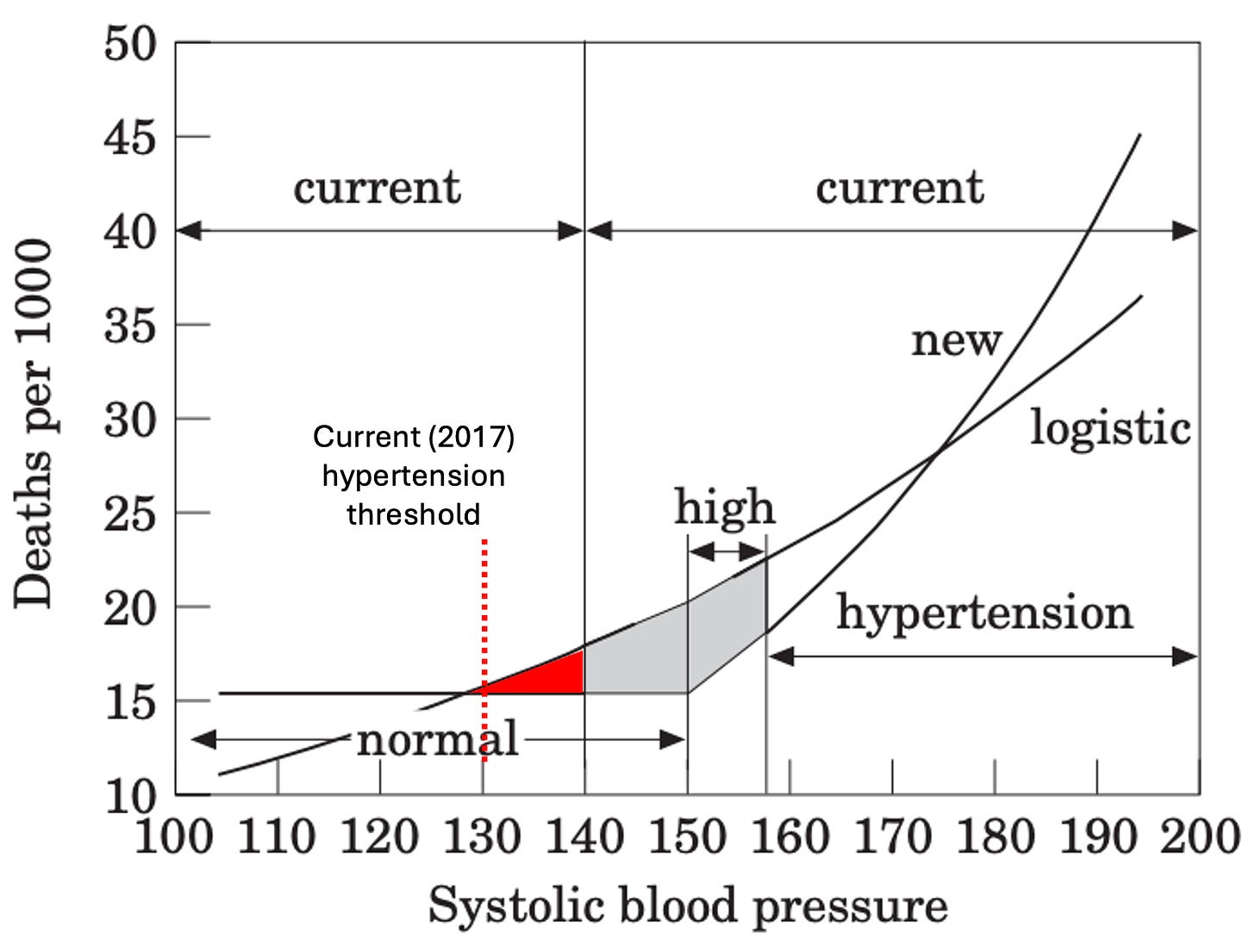
Note: when this (forgotten) paper was published, the conventional blood pressure thresholds were less aggressive. I modified its graph to match the current guidelines.
After the paper was published, it was mostly ignored but eventually received this response (which again illustrates how resistant medical dogmas are to evidence that refutes them):
The National Institutes of Health’s National Heart, Lung, and Blood Institute (NHLBI) issued a statement regarding Port’s findings saying that they found it “thought provoking” but “After careful review of this study, the NHLBI finds that it does not offer a basis for changing the current hypertension guidelines.”
This is a shame because the same results have been found with more modern technologies. For example, consider the results of this study of 415,980 patients obtained through their electronic health records which again shows rather than being linear, an age dependent threshold exists which is not at all recognized by the guidelines:
Note: in addition to a SBP below 130 significantly increasing the chance of death, this study also found a DBP below 80 (a common consequence of blood pressure medications) made them 8-19% more likely to die. Furthermore, another smaller study of 800 adults over 60 found a DBP under 80 made participants 90-190% more likely to die and that a SBP under 120 was again associated with a higher risk of death.
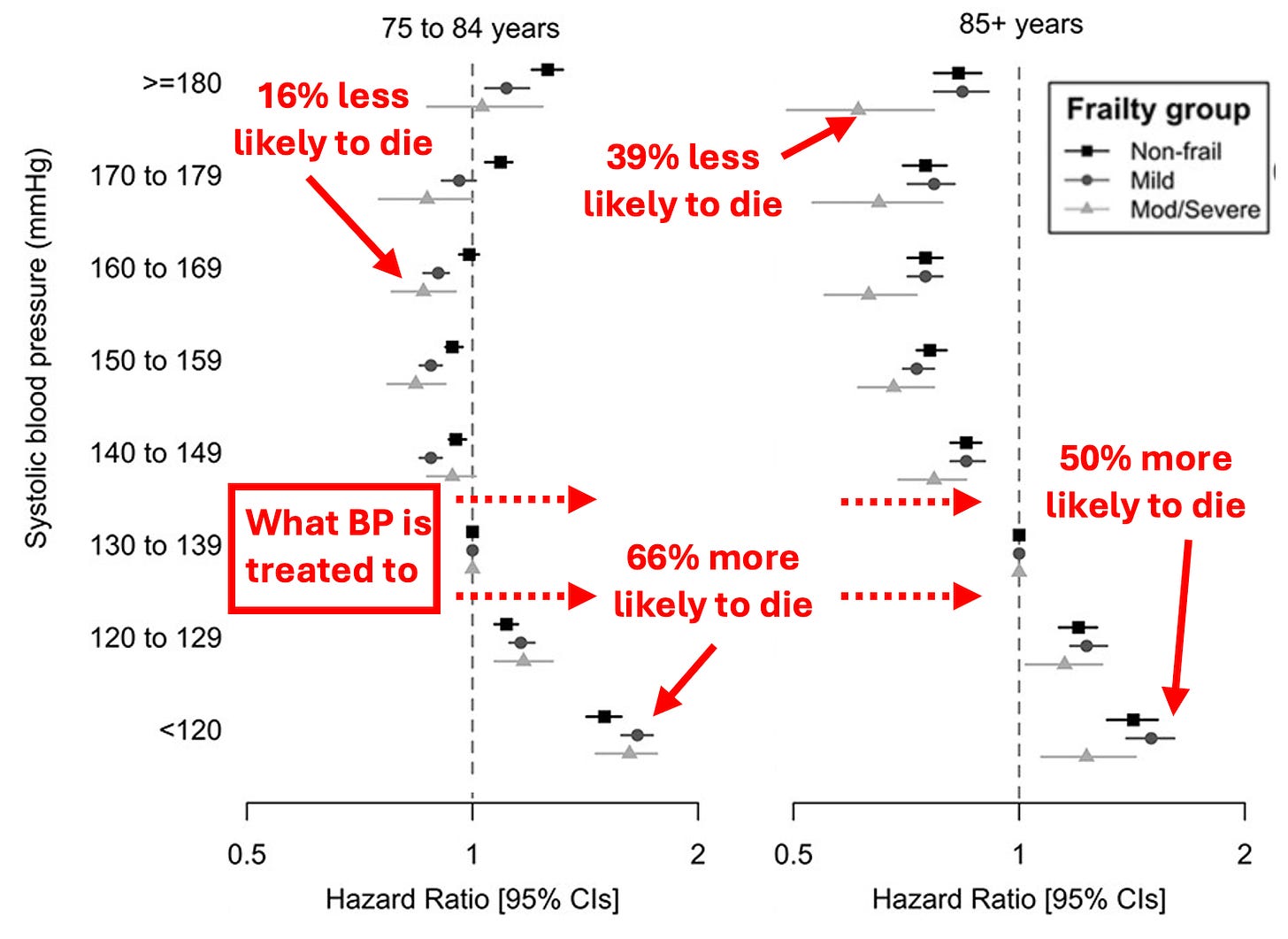
Since less elevated blood pressures are more common than the higher ones, each time the treatment target is lowered by a small amount, it results in a large number of people getting started on the drugs, especially for the elderly (since their blood pressure rises to compensate for the decreased health of their arterial system).
Because of this, a large number of people are diagnosed as having dangerous hypertension in the linear model but not in the more accurate threshold model. The author of the 2000 paper hence tried to illustrate that point:
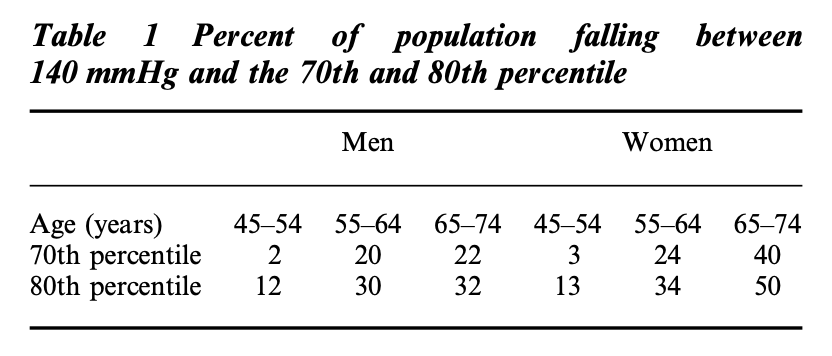
Sadder still, these numbers are even vastly worse when 130 is set as the threshold instead of 140 (which is what happened in 2017). For example, 77% of adults over 64 meet this threshold and 79% of those over 74 do.
Blood Pressure Mortality Studies
Given the hype around blood pressure, you would assume it had been clearly proven lowering blood pressure improved survival. Unfortunately, as best as I can tell, those studies don’t exist and instead a universal assumption exists that lowering blood pressure is good and hence that if a drug can lower blood pressure, it must be good and should be approved for the market.
One of the most pivotal moments began in 1973, when due to no studies existing that proved lowering a moderately elevated blood pressure reduced one’s chance of dying, a massive, decade-long, public study was conducted in the United Kingdom where 700,000 people were contacted, and ultimately 17,354 patients between the age of 35-64 years of age who had blood pressures below 200 (averaging 158/98 in men and 166/99 in women) were selected to take a beta blocker, a thiazide diuretic or a placebo.
It found that treating these high blood pressures made no real difference in the likelihood of a coronary event (e.g., a heart attack), as the rate was only reduced from 5.5 to 5.2 per 1000 patient-years, and there was likewise almost no difference in the death rate (253 deaths vs. 248 deaths—which worked out to a 0.06% reduced chance of dying). However, the study did show lowering blood pressure made someone less likely to experience a [likely hemorrhagic] stroke (as there were 18 fatal and 42 non-fatal strokes in the treatment groups vs. 27 fatal and 82 non-fatal in the placebo group), which led to a small overall reduction in those strokes (roughly one stroke delayed for around nine hundred years of treatment).
Additionally, significant side effects were frequently seen in the trial (roughly 25% left):
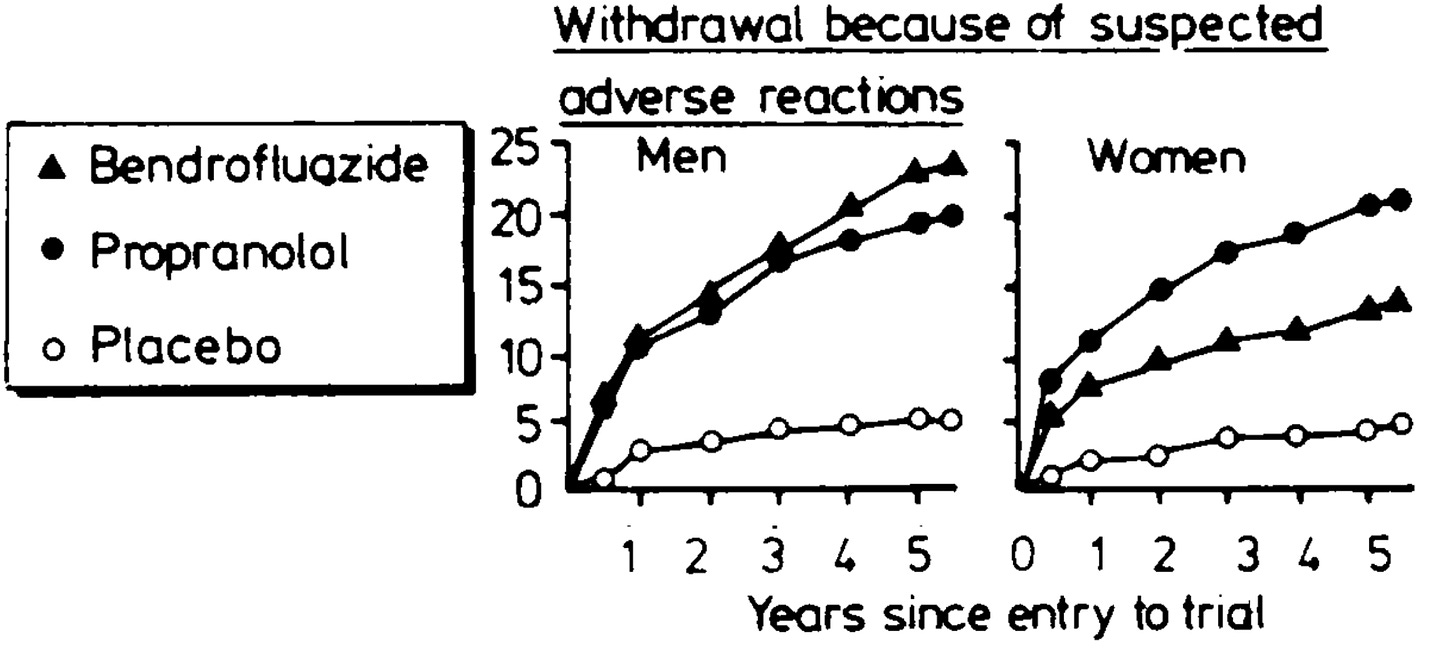
Once this trial happened, “heart disease” was changed to “cardiovascular disease,” thereby making it possible to create the perception that treating blood pressure stopped heart attacks while simultaneously concealing the actual benefit—a small reduction in vascular strokes.
Note: in a recent article, I detailed another consequential example of these linguistic tricks. basal cell carcinoma (which is quite common and caused by sunlight exposure) is never fatal, whereas melanoma (which is rarer and caused by a lack of sunlight exposure) is often very dangerous. The label “skin cancer” was applied to each to create the perception sunlight was deadly, when in reality it prevents you from dying of cancer.
Much later, a 2009 Cochrane review (considered the gold standard for evaluating scientific evidence) was conducted which found that very little benefit (a 1-12% reduction in a few key symptoms or the risk of death) was seen from lowering SBP below 135 compared to having it below 140 and that this benefit was likely outweighed by the margin of error created by unclear data and significant side effects in the trials. These results were confirmed by a 2020 Cochrane Review which again found a negligible benefit from the aggressive blood pressure lowering targets which was outweighed by the harms those drugs created.
Note: these reviews also found a small increase in kidney disease (e.g., acute injuries or chronic kidney disease), which makes sense since the kidneys are damaged by insufficient blood reaching them, and is unfortunate since kidney disease creates heart disease and raises blood pressure.
This in turn may help to explain why there has been such a strong focus on the theoretical benefit of lowering blood pressure rather than actually proving it exists.
Changing Guidelines
When the blood pressure craze took off, there was a rush to bring the blood pressure lowering drugs to market before their benefit was actually proven (outside of a few short term studies which showed a small benefit for people with very high blood pressures). That mindset in turn has defined this field, so as the years have gone by, without evidence to support it, the blood pressure thresholds keep on getting lowered and more and more people are being put on these medications. Because of this, roughly 60 million American adults (23%) take these medications. This is particularly unfortunate for the elderly as due to their calcified arteries, they both have the least ability to tolerate insufficient blood pressure and simultaneously are the most likely to have elevated blood pressure.
My best guess is that this inexorable march to putting everyone on these drugs is due to some combination of the following:
•Research funding is available for these areas (e.g., from the drug manufacturers) hence being a safe area of research for academics to explore.
• It illustrates the “if you have a hammer, everything looks like a nail” phenomenon and the medical profession’s desire to find more justifications for using its tools (especially since humans tend to double down on their existing approach when it fails rather than consider a new one).
•”Experts” on guideline panels are paid to create recommendations that result in more and more people taking the drugs, a sadly common phenomenon in medicine (e.g., in a recent article I conclusively showed how this happened with the statins).
Let’s now look at how the guidelines have changed over the years.
Note: as these guidelines show, originally the focus was on treating diastolic blood pressure under the belief the heart had to “work harder” if there was too much blood in the circulation. I believe this is helpful to note since it was believed for decades (but now is not) and hence illustrates how arbitrary many dogmas are.
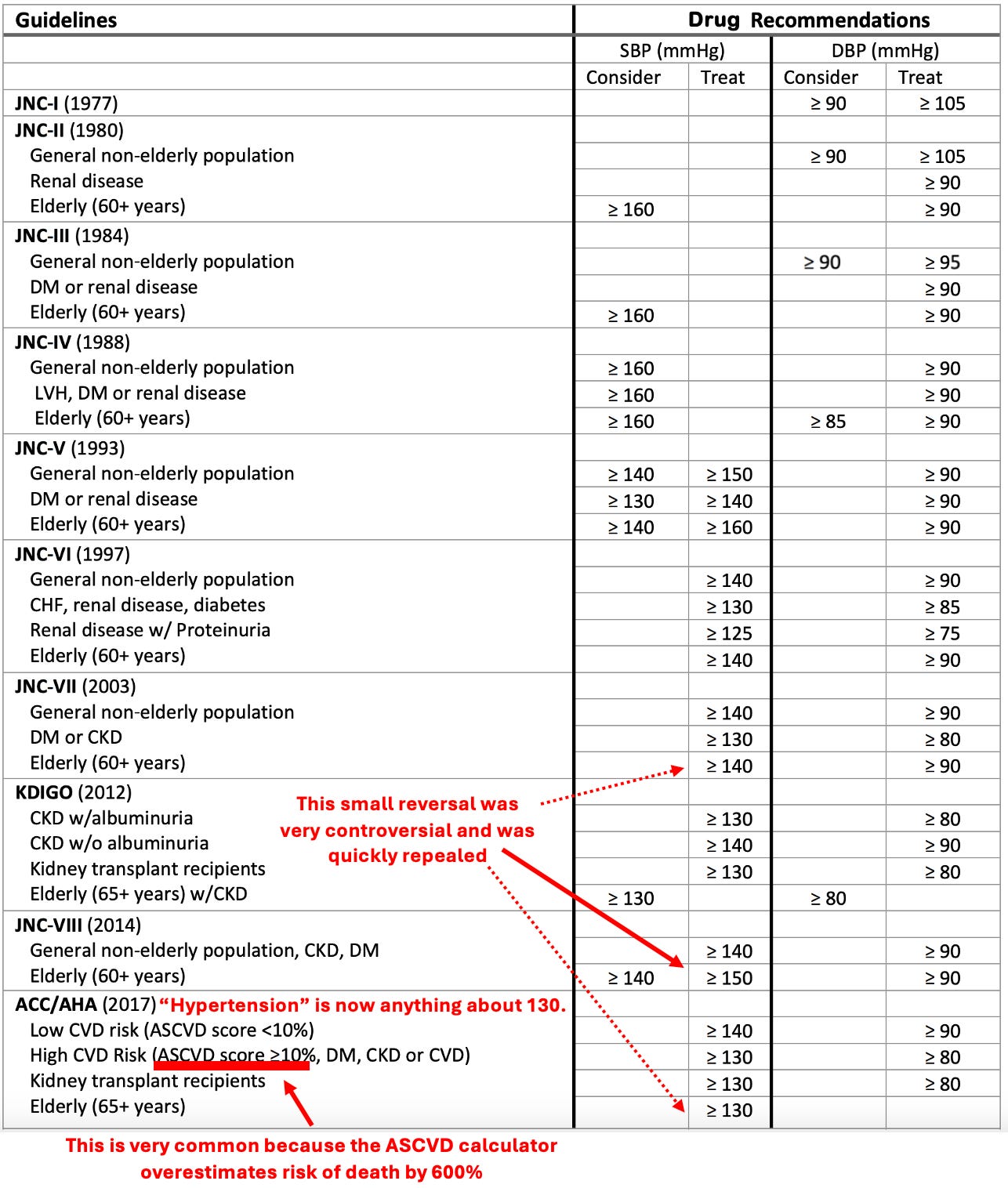
To quote the 2017 guidelines:
Rather than 1 in 3 U.S. adults having high blood pressure (32 percent) with the previous definition, the new guidelines will result in nearly half of the U.S. adult population (46 percent) having high blood pressure, or hypertension.
Note: this rate further increases with age (e.g., 79% of men and 85% of women over 75 now have hypertension, while 71% of men and 78% of women now meet the threshold to start blood pressure medications).
Secondary Effects of Hypertensive Medications
In many cases, the actual mechanism of a drug greatly differs from the purported one. For example, statins are sold on the basis that cholesterol causes heart disease and they lower cholesterol. However, as I showed in a recent article, there is very little evidence cholesterol causes heart disease, and more importantly, prior to the statins hitting the market, there was no mortality benefit shown from the other cholesterol lowering medications. In the case of the statins, a very small benefit has been shown (living a bit under 3-5 days longer if you take them for 5 years) and this is likely due to their anti-inflammatory and anti-clotting properties, both factors known to prevent heart attacks.
In the case of blood pressure medications (which each work in a different manner), very different degrees of benefits are seen from their use despite them creating the same drop in blood pressure. This in turn strongly argues that their benefits are not due to them lowering blood pressure, but rather how each one specifically affects the body. To illustrate:
•A 1997 paper in JAMA reviewed the literature and found significantly different benefits from the antihypertensive drugs depending on which type was used.
•A 1998 review found that the (known) cardiovascular benefits of ACE inhibitors were not seen with calcium channel blockers, despite the latter having a more significant effect on blood pressure.
•A 2000 study of 3577 diabetics found that a specific ACE inhibitor, despite minimally reducing blood pressure (a 2.4 reduction in SBP and 1.0 reduction in DBP) had a massive effect (a 25% reduction) on the risk of a heart attack, stroke or cardiovascular death.
•A 2007, eight year long (and NIH funded) double blind study of 42,418 subjects found that when two different types of blood pressure medications were used, there was no difference in their effect on blood pressure but simultaneously, found their rate of preventing heart failure varied by 18% to 80% depending on the drug, leading the investigations to conclude: “blood pressure reduction is an inadequate surrogate marker for health benefits in hypertension.”
Harms of Hypertensive Medications
The typical management of blood pressure is to use a combination of drugs until they collectively achieve the desired blood pressure and simultaneously to switch out drugs that cause too many side effects for the patients to tolerate them.
This is a problem because as the previous section showed, the drugs have very different effects on the body and should each be considered on the basis of whether their individual effects are appropriate for the individual patient’s situation rather than whatever reaches the desired blood pressure—but as that would get in the way of drug sales it never happens.
Typically, the most common side effect of blood pressure medications are complications of poor perfusion. For example, blood pressure medications increase the risk of fainting by 28% and are notorious for causing older individuals (who have calcified arteries and hence difficulty getting blood to the brain) to become lightheaded and then suffer falls that can be devastating.
To illustrate, a 2014 JAMA study of 4961 adults over 70 with hypertension compared 14.1% who received no antihypertensive medications, 54.6% who were on moderate-intensity medical therapy, and 31.3% on high-intensity medical therapy. They were monitored for three years, during which 9% experienced falls, and 16.9% died. When falls were looked at, those in the moderate-intensity treatment group were 40% more likely to have a fall that caused a serious injury, and for those with a previous fall history, the moderate-intensity group was 117% more likely to have a serious fall, and the high-intensity group was 131% more likely to have a serious fall (which begs the question why they were still on those drugs). The authors unfortunately did not report the rate of death between the groups but did find that calcium channel blockers had the highest rate of causing falls.
Note: in 2007, an important Israeli study was conducted that found that discontinuing an average of 2.8 drugs per elderly patient reduced their 1-year death rate from 45% to 21% and hospitalization rate from 30% to 11.8%. While the exact data was not shown in the study, I am fairly sure a significant degree of the benefit was from removing unnecessary anti-hypertensives, as this is a core principle in geriatrics.
Similarly, Emergency Medicine has recognized that it is unwise to aggressively treat blood pressure in the Emergency Department due to the risk it will cause an ischemic stroke in the brain due to insufficient blood flow in the brain. To quote one review paper on this subject:
Most ED patients with SBP ≥180 mm Hg or DBP ≥110 mm Hg have elevated BP without evidence of end-organ injury…There are no evidence-based thresholds at which asymptomatic but markedly elevated BP in the ED benefits from immediate reduction [and] these patients have no immediate indication for rapid BP lowering.
Given the aforementioned variability in clinical practice, it is not surprising that the majority of IV medications given to achieve immediate BP reduction in the ED are done so inappropriately to patients without new or worsening end-organ injury that can be modified by rapid treatment…rapid BP reduction can cause significant harm by impairing cerebral blood flow, and it has not been shown to improve clinical outcomes except in hypertensive emergencies
For time-sensitive conditions such as acute ischemic stroke, rapid BP lowering may be indicated when BP exceeds 185/110 mm Hg and thrombolytic or endovascular treatment is planned. Most acute ischemic stroke patients, however, are not candidates for thrombolytic or endovascular therapy, and BP lowering should be avoided. The ischemic penumbra lacks autoregulation of cerebral blood flow and is dependent on systemic perfusion pressure, such that acute lowering may worsen ischemia.
Many other more serious diseases also result from low blood pressure, especially in the organs most sensitive to a loss of blood flow. For example, low blood pressure is strongly linked to cognitive decline (since the brain needs adequate blood to function). Likewise, as you lower the blood pressure the kidneys start to struggle as they require sufficient blood flow to function. For example, hypertension drugs increase the risk of an acute renal injury by 18%, and in patients who have end stage renal disease, when those with blood pressures below 130 were compared to those with ones between 130-149, those with lower blood pressure were 38.9% more likely to die.
Finally, when one’s blood pressure is below 90, it is diagnosed as “hypotension.” The most common symptoms of hypotension are lightheadedness or dizziness. Other common symptoms include: fainting (when it gets lower), blurry vision, confusion, nausea or vomiting, sleepiness, fatigue, and weakness. Given the high inaccuracy of blood pressure measurements and the patients often being put on excessive hypertensive medications (especially as they age and the body is less able to handle low blood pressures), these symptoms affect many blood pressure medication users to varying degrees.
Note: in critical care medicine, blood pressures below 90 are viewed as dangerous because organs do not get enough blood, which is unfortunately, since blood pressure medications are generally found to develop one’s risk of developing hypotension.
Additionally, each blood pressure medication works differently. On one hand, this is a good thing because it allows each of them to exert unique therapeutic benefits independent of their effect on blood pressure, but on the other hand, it means they each have unique side effects.
Presently, four main types of antihypertensive drugs exist:
1: Diuretics (the oldest): These drugs lower blood pressure by increasing urination by blocking the reabsorption of sodium in the kidneys. Many different types of diuretics exist with slightly different side effect profiles and different electrolytes they affect, but generally, these drugs:
•Cause a wide range of symptoms from electrolyte imbalances, particularly of sodium and potassium (e.g., low sodium levels are a common cause of weakness and hospital admissions, while low potassium affects 8.2% of users—occurring at a rate 973% greater than those not on the drugs).
•Cause many of the side effects associated with dehydration (due to them effectively dehydrating you) such as stomach issues.
•They (depending on the class) can sometimes create sulfa sensitivities or allergies.
•They cause many of the general effects associated with low blood pressure (e.g., lightheadedness).
•Some of them (ie. the thiazides) also increase uric acid levels, which may explain why these drugs increase the risk of diabetes or why they cause a 358% increase in the risk of gout (which affects 2.0% of users).
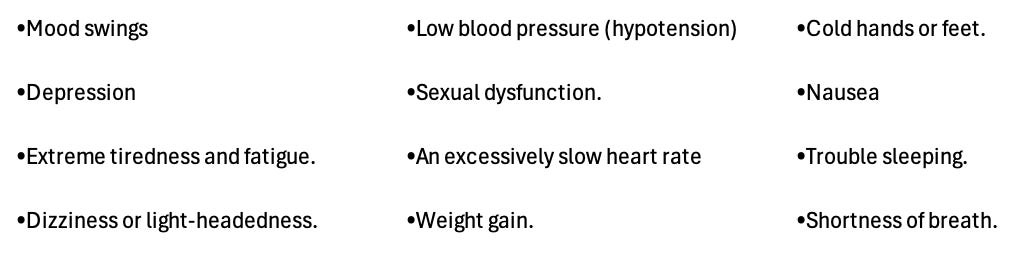
2: Beta-blockers: These drugs slow the heart and make it pump less forcefully. This is found to be very helpful for heart failure patients, but simultaneously has a variety of common side effects such as constricting the peripheral arteries. Typically, patients have the greatest difficulty tolerating beta blockers and frequently report a worsened quality of life from them (which doctors sadly often don’t recognize). Some of their most common side effects include:
3: Calcium channel blockers: These reduce the force of contraction of the heart, dilate arteries by relaxing the smooth muscle in them, and somewhat slow the heart rate. The major issues with these drugs are that they cause edema (swelling) throughout the body (affecting between 5.7-16.1% of users depending on if a low or high dose is taken) and frequently cause dizziness, lightheadedness, or constipation. These drugs are often quite helpful for resetting an abnormal heart rhythm, but also can cause other symptoms such as tiredness, headaches, abnormal heart rates, and shortness of breath.
4: ACE inhibitors (and related medications): When the kidney does not have enough blood, it releases a hormone that sets off a cascade within the body to raise blood pressure. ACE inhibitors in turn block that cascade—which can often be quite helpful as parts of the cascade can be damaging to the body. The most common side effect associated with these drugs is a chronic dry cough (which patients often develop over time as they become sensitized to the drugs—with estimates of its frequenty ranging from 3.9% to 35% of users—e.g., this detailed review determined it was 8.0%). Other common side effects include headaches, lightheadedness, and a loss of taste.
Three of the more concerning effects are a 26% increased risk of acute kidney injuries (which affect 1.5% of users—including a few people I know), a 103% increased risk of hyperkalemia (which can be quite dangerous and affects 4.8% of users), and a 19% increase in the risk of lung cancer.
Note: A variety of other less appreciated side effects from these drugs also exist (e.g., they increase one’s risk for lung cancer by 19%, and while they are typically thought to protect the kidneys, I’ve seen a few patients who instead developed renal failure from them—an effect which is somewhat acknowledged within the medical field). For those interested, a more detailed summary of the rates of their side effects can be found here.
Under Recognition of Side Effects
While the numbers I just showed are quite concerning, I believe they actually underestimate the rate of side effects as much of that data comes from industry clinical trials which deliberately finds ways to downplay their drug’s side effects. Because of this, I believe independent patient survey’s provide a far better perspective on the rate of symptomatic side effects. Consider for example this 1995 Survey in Sweden which found roughly 1 in 5 users experience side effects:
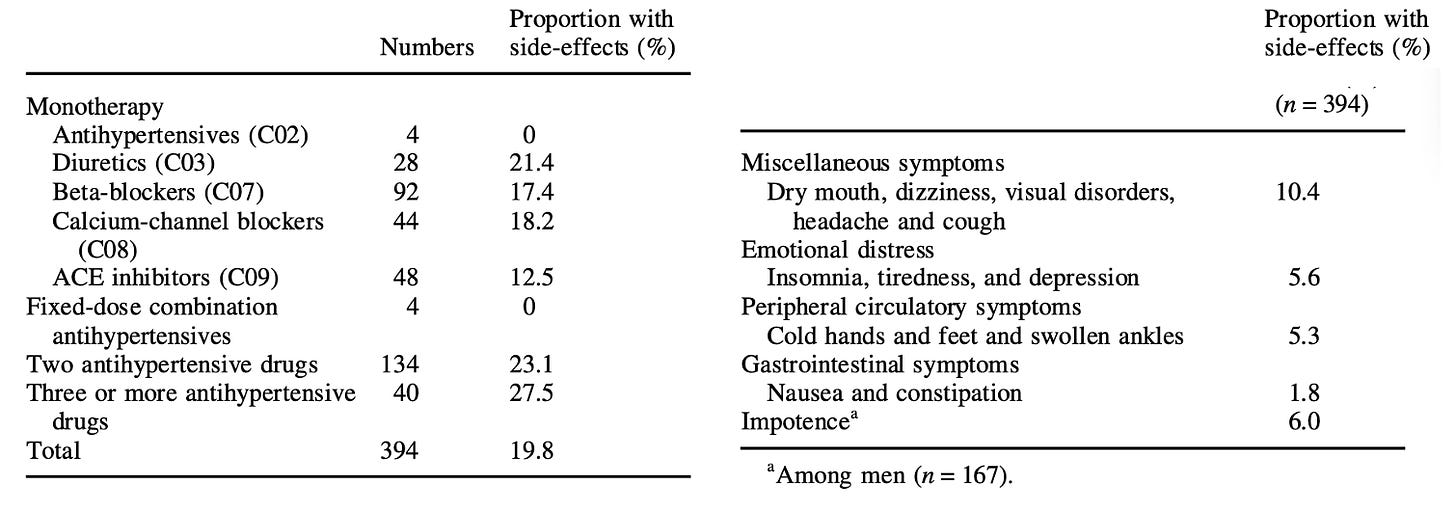
Because to these side effects, patients frequently stop taking antihypertensives. For example, a study of 370,000 patients under 65 between 2007-2014 found 23.5% stopped taking the drugs within 270 days of starting them, while 40.2% of those who continued often skipped the medications.
Note: large studies have found patients are the least likely to stop using ACE inhibitors (and the related ARBs) and the most likely to stop using beta blockers or diuretics (especially beta blockers), something congruent with the rate of side effects we observe in practice.
Given such a high discontinuation rate of the drugs of the surprising things about blood pressure drugs is how little awareness exists regarding their side effects, especially amongst doctors (e.g., the article I just cited acknowledged side effects were a reason for discontinuation but instead emphasized it was due to patient ignorance about the importance of the drugs). All of that was best shown by this 1982 study (which would not be repeated in today’s political climate) compared how patients, their families and their doctors felt about the effects of these drugs on them. It found:
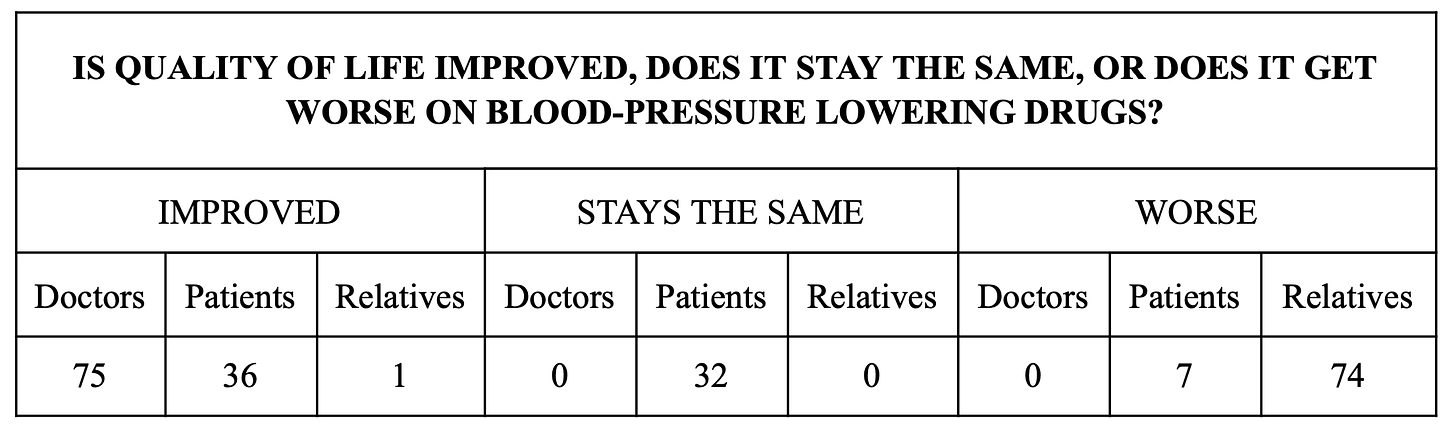
Note: of these patients, 48% received beta blockers, 25.3% received beta blockers and diuretics, and 12% received diuretics only. In the surveys relatives completed, 25% characterized the worsening as mild, 45% as moderate, and 30% as severe, with the most commonly cited deteriorations being an undue pre-occupation with sickness, irritability and a decline in energy, general activity or sexual activity.
Salt
Finally, while it is not a drug, aggressive salt lowering is frequently advised to patients. I personally do not support this approach since:
•As mentioned before, significant salt reduction has almost no effect on blood pressure. Furthermore, something many people don’t consider is that patients in the hospital are routinely given large amounts of IV sodium chloride, in many cases receiving ten times the daily recommended sodium chloride we are supposed to consume. Despite this, their blood pressure does not rise.
•Low sodium levels are strongly correlated with a risk of dying (e.g., the salt consumption target we are recommended to follow increases one’s risk of dying by 25%). Likewise, a common reason for hospital admissions is symptoms resulting from low sodium levels (as once they get too low, they can be very dangerous), and 15-20% of hospitalized patients have low sodium levels at admission
Note: I presently believe many of the associations between salt and heart conditions are due to the zeta potential destroying aluminum processed salt often contains as a desiccant—something not for example found in natural salt products or IV saline given at hospitals. Conversely, I believe many of the benefits from hospital care are a result of IV fluids being routinely given as they somewhat restore the physiologic zeta potential.
Treating Hypertension
Virtually every awake physician I know gradually reached the conclusion that the current hypertension paradigm was flawed and hence became much more conservative when they would directly treat blood pressure while simultaneously having a large focus on reversing the causes of high blood pressure rather than trying to treat it with medications. Nonetheless, there are still cases where treating hypertension has merit, and in the final part of this article, I will try to illustrate those, along with what I believe to be the safest conventional options, and our preferred natural options for treating blood pressure (which typically are all that’s needed).