How Stressed is the NHS?
Sun 10:37 am +01:00, 15 Nov 2020
My top doctor friend has been pouring over the NHS’s latest data. He’s not convinced the NHS is under nearly as much pressure as the Chief Scientific Officer and Chief Medical Officer suggested in the run-up to the second lockdown.
When is a Covid Patient not a Covid patient?
On November 12th the NHS released a monthly summary of COVID hospital data.
I was hoping it might answer my key questions:
- • How many patients reported as admitted every day from the community actually have Covid symptoms?
- • How many patients reported as Covid inpatients are in hospital because they are ill with Covid rather than simply testing positive as a consequence of routine testing and are asymptomatic?
- • How many patients caught Covid while in hospital having been admitted for other reasons – i.e., the rate of hospital-acquired infection.
- • What is the average length of stay of a Covid patient?
The first two questions address the possibility that we could have a ‘casedemic’ rather than a genuine second wave pandemic. The third question on hospital-acquired infection rates goes to the issue of whether admitting symptomatic Covid patients into general hospitals might be making the problem worse. The last question informs assessment of the burden of care on the NHS and whether predictions of the system becoming overwhelmed absent a lockdown were credible.
I’m going to work through a couple of examples to illustrate just how difficult it is to answer these questions using the figures presented by the NHS and reported on the TV. Apologies if this is a bit dense and difficult to understand, but it’s important.
Take November 4th.
The categories of figures presented by NHS Statistics are as follows
Number of patients admitted with Covid in last 24 hrs: 296
Of that number, 113 (38%) were under 65 years of age (lower risk). It isn’t clear whether these 296 patients were admitted with symptoms of Covid and a positive test result, but for the purposes of the exercise we will assume so.
Total number of inpatients diagnosed with Covid within previous 24 hrs: 1,001
It’s clear that the number of patients with positive tests on arrival to hospital is much lower than those who test positive while in hospital. We aren’t told when the patients diagnosed in hospital had their swabs taken – because patients are swabbed multiple times in hospital.
In the October monthly round up, there were different categories of swab dates, so it was easier to figure out which patients had become Covid positive while in hospital and when they became positive in relation to the date of admission. In November, these columns have disappeared. I don’t understand why we aren’t allowed to see that information this month, because it’s an important indicator of the rate of in-hospital infection.
NHS management argues that even an asymptomatic Covid patient imposes a greater burden on hospital staff because of the need to shield staff and other patients. There is justification for that view, but it does not explain why this information is kept from the public. Concealing such data just reinforces suspicion and fosters a lack of trust in the system – precisely the opposite of what’s needed.
Discharges total: 977
Whenever one hears Covid inpatients discussed on TV, there is never any reference to patients getting better and being discharged from hospital. In fact the overwhelming majority of patients in hospital for COVID are only in hospital for a few days and are then discharged home.
Further, in the slide deck leaked last week there is a reference to the NHS investigating the possibility of providing care at home to Covid patients rather than admitting them to hospital – I wonder why that is?
Could it be a clandestine acknowledgement that there is a serious problem with in-hospital cross-infection control? Graph 1 shows that the rate of discharges of COVID patients is much the same as the rate of in-hospital diagnoses. So, if the NHS could get on top of the estimated 20% of self-generated hospital-acquired infections by only admitting the seriously ill, it might relieve pressure.
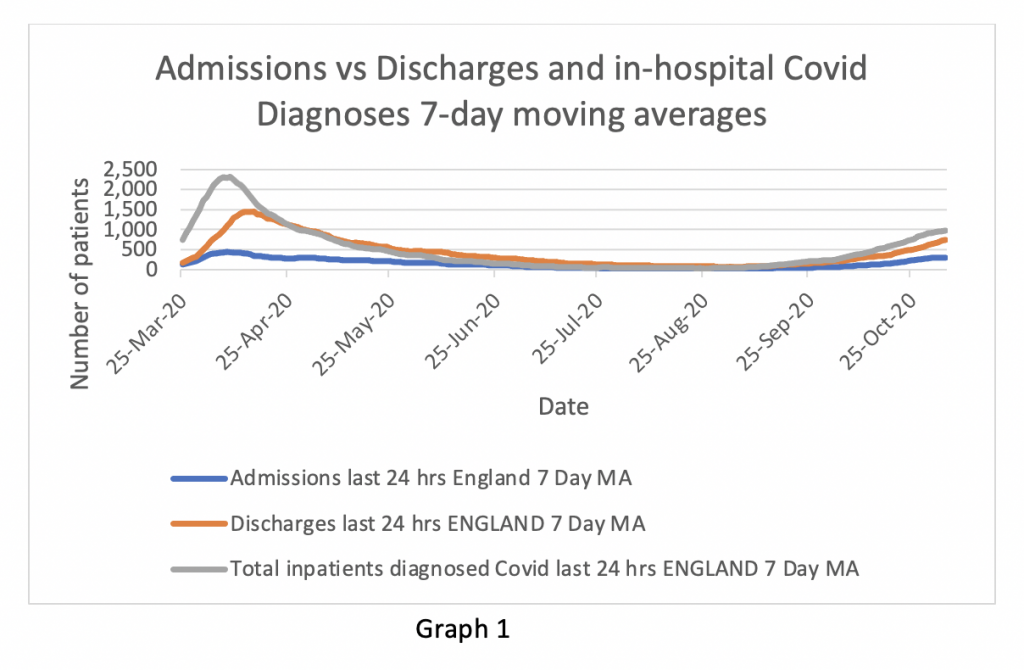
Covid ICU patients: 986
On November 5th there were 986 patients in English ICUs suffering from Covid-related symptoms out of a total of 3,291 ICU patients – about 30%. That’s a significant percentage of the total. Numbers in ICU tend to mount up because patients often stay a long time – and the sicker they are, the longer they stay. The average length of ICU stay for survivors is five days and for non survivors eight days (ICNARC report).
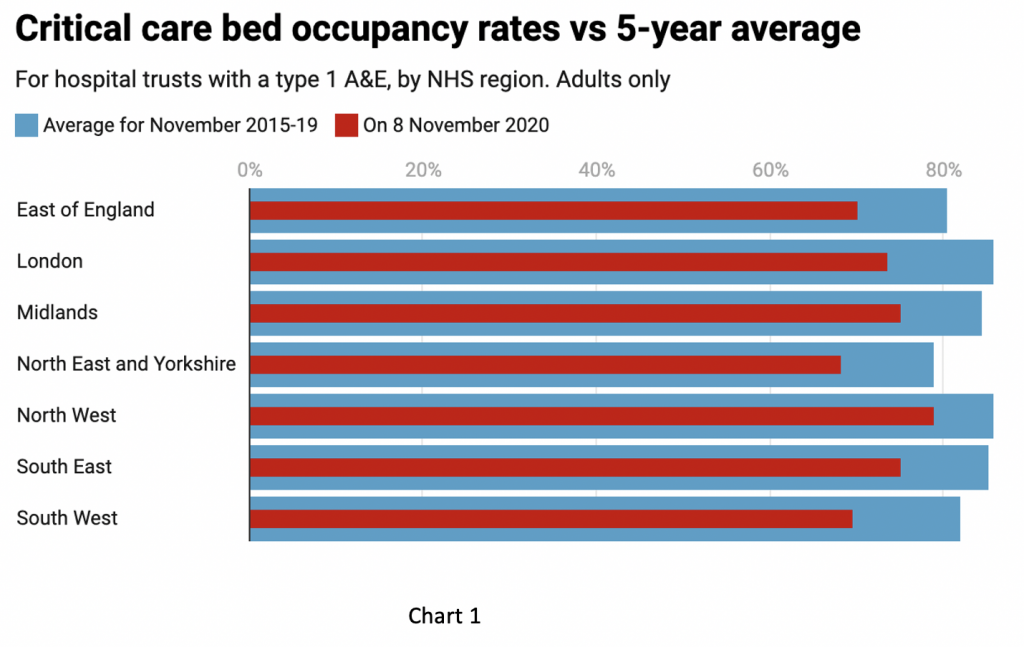
What the new data does not say – but the leaked NHS slide deck reveals – is that there was substantial spare ICU capacity still available in the system as of November 1st, with bed occupancy running at an average of 78%. This has been flagged up by the helpful graphic from the Spectator Covid tracker (Chart 1). It is important to recognise that the NHS has expanded its critical care capacity since the spring and most trusts have put in place escalation plans where normal ward beds can be converted to higher intensity care to meet rising demand – prudent preparation. So, when the figures suggest spare capacity on a percentage basis it’s true to say that overall capacity has increased since last year. The fact that such plans have been put in place ought to mitigate exaggerated predictions of impending doom in favour of more measured and nuanced advice to policy makers.
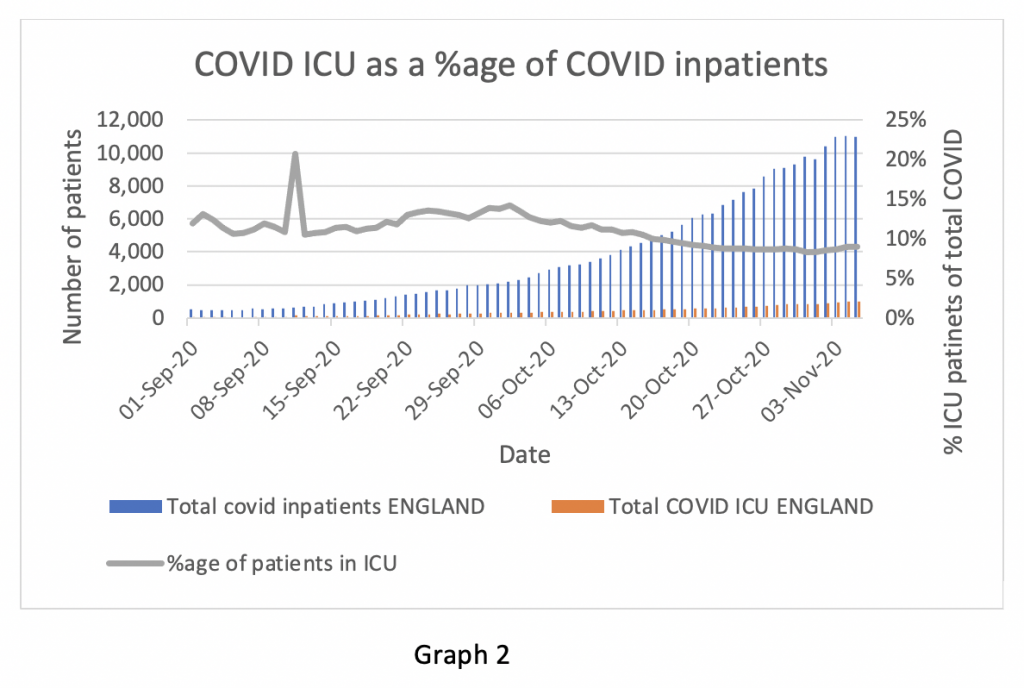
The proportion of Covid patients admitted to ICU has fallen from 12-13 % to 8-9%. There are several possible reasons for this, all of which may play a part. Some hospital doctors have suggested that the disease is not as severe as it was in the spring. Treatments such as high dose steroids and anti-coagulants administered early in the course of the disease may reduce the proportion of patients needing ICU care and shorten hospital stays. In addition, there may be measurement artefact if substantial numbers of patients recorded as suffering from Covid do not in fact have the disease (false positives) or may be positive for Covid but are in hospital for other reasons and do not have Covid symptoms.
(Graph 2 – NB the spike in early September is a recording error in the data and can be ignored).
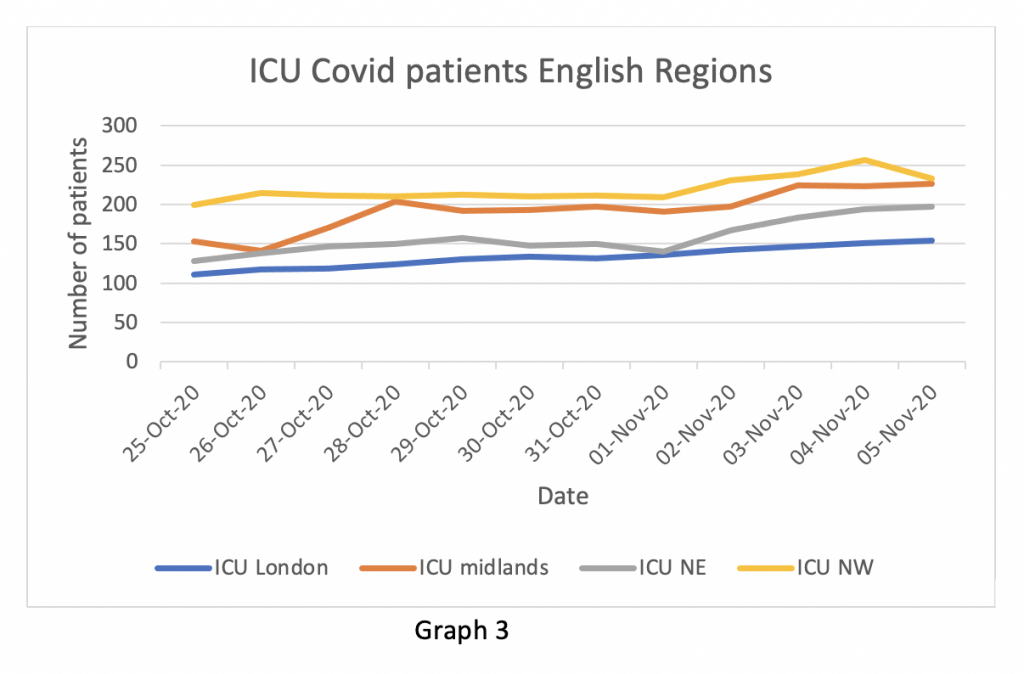
In the two weeks up to November 5th, the number of ICU patients in the worst affected English regions was essentially stable with the exception of the Midland region which had seen a significant increase, recently levelling off – note these figures were known to the NHS before the Parliamentary lockdown vote on November 4th but to my recollection not referenced in any of the alarming public briefings. The other English regions had negligible numbers of Covid ICU patients – not worth recording on Graph 3.
Chris Hopson (CEO of NHS Providers) has criticised using ICU occupancy as a measure of Covid pressure on the basis that acute ward pressures are a more representative measure of the stress. That’s a reasonable point, but he forgot to address the revelation from the leaked slide deck that oxygen utilisation by trusts is no higher than normal at this time of year, and although there undoubtedly is pressure on hospitals in the North of England, the NHS is managing it. Hopson’s extraordinary argument that the entire population should remain under indefinite house arrest so that the NHS can continue doing elective surgery surely tests the extreme limit of deformation professionelle.
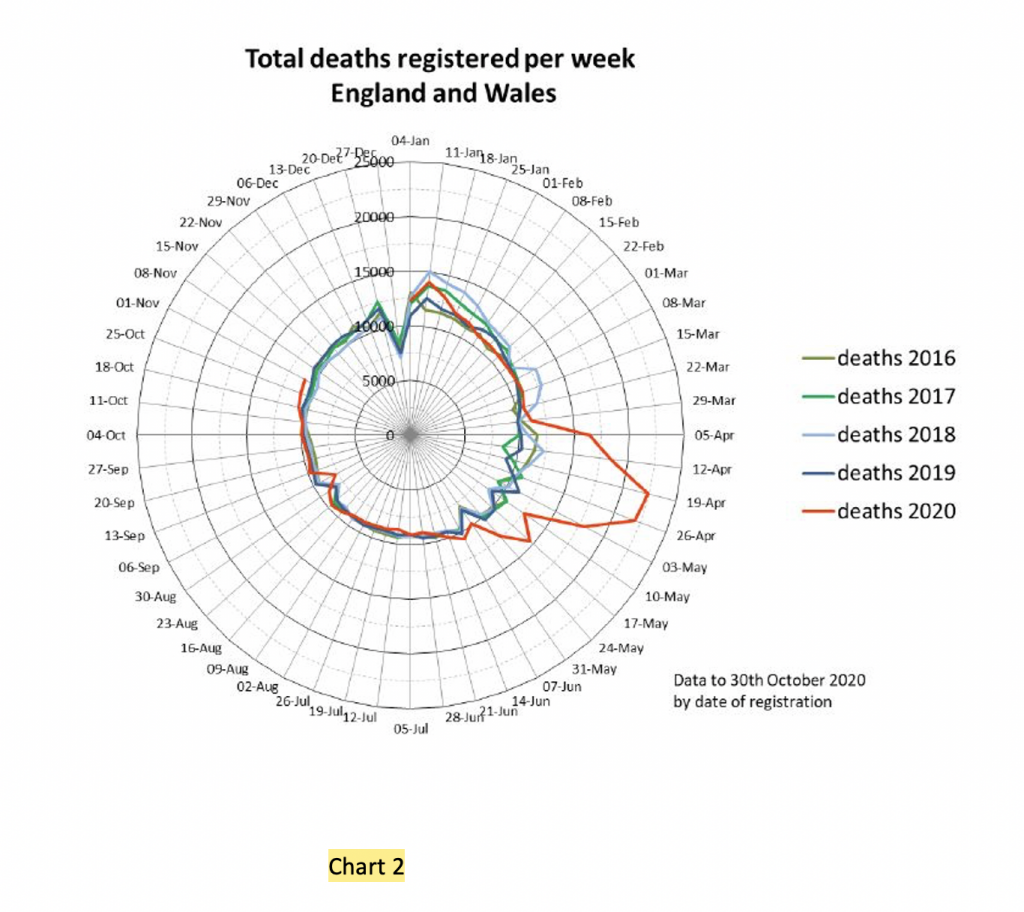
Finally, where are the deaths? True, there’s a time lag between community infection, hospitalisations, ICU stays and deaths. But one would have expected to see a rise in deaths by now – and it hasn’t happened (Chart 2). The tiny increase in deaths to October 30th is all due to deaths at home – there are no excess deaths recorded by the ONS from respiratory disease.
For clarity, I should say that Covid is a nasty infection. It can make people very ill and sometimes die. I certainly hope I don’t get it. That said, I think I’m sufficiently informed about the risks to make up my own mind with respect to sensible and proportionate precautions – and my fellow citizens are, too.
I’m sure the answers to the questions posed in my opening paragraph are known to NHS executives. If they do not know the answers, they really ought to. When they do know, the information should be made available to Members of Parliament and the public without spin or exaggeration.
I have little doubt that senior NHS managers will take the view that I have no right to be shown all the information that informs their decisions or advice to Government. That the public should just obediently take instruction on trust and comply with Government recommendations indefinitely without asking impertinent questions. I don’t accept that, obviously. If it is necessary for my freedoms to be curtailed, I require a full explanation. I expect complete disclosure of the information behind such recommendations and it should be open to interrogation by experts not affiliated to the Government machine. I expect the restrictions to be publicly reviewed on a regular basis. I take great exception to the view expressed to the Parliamentary Science and Technology Committee by Sir John Bell, Regius Professor of Medicine at Oxford, that if the public “behave themselves” then some “freedoms may be restored”. On what basis does this man presume such authority over others?
All of this goes to the issue of whether Parliament was properly informed before the lockdown vote. For what it’s worth, I don’t think the data I’ve seen supports the conclusions drawn by decision makers and their advisors. I readily concede I am not an expert in infectious disease epidemiology, but I am a reasonably well informed medical professional with over 30 years clinical experience. If the experts can’t convince me of the need for a full lockdown, their argument is in trouble. Even the BMJ is pushing back against the concealment of information and repression of open debate (see above).
If Members of Parliament were not provided with adequately contextualised information before the lockdown vote – and that information was readily available in the NHS – that’s a scandal. We should be far more worried about that than we are about the virus.
Finally, I note the following from an article in the Financial Times dated November 13th:
NHS Providers said in a letter to Mr Sunak that if his review on November 25th failed to allocate the necessary money for 2021-22, “the health and wellbeing of hundreds of thousands of . . . patients is at risk”.
I’m sure I’ve heard that before somewhere.
By
https://lockdownsceptics.org/