Here is a Coronavirus puzzle for you to ponder – A guest article
Sat 10:05 am +01:00, 11 Jul 20209th July 2020
A guest article
I was sent this piece on Vitamin D and COVID by a reader of this blog. I thought it was very good and asked them if they minded me posting it. They said fine, but they wish to remain anonymous. Not everyone likes the glare of publicity – with all the attending Trolling and insults that inevitably follow [you should read my in-box sometime].
Season, Latitude, and COVID-19 Severity
Here is a coronavirus puzzle for you to ponder. For context, let’s look at how many people have died of COVID-19 in the USA (as of mid-June). Websites give different totals, but it’s around 120,000, or about 360 per million of population. So how many died in Australia? 102. How many died in New Zealand? 22. In both countries, the death rate is 4 per million. That is an extraordinary contrast!
Wouldn’t public health officials like to know the cause of this difference? Are the Antipodeans that much better at hand-washing and social distancing than the people of New York, Italy or Great Britain? Do they share a highly-effective cure kept secret from the rest of the world? Or is there another reason for the disparity?
Unlike the USA and other countries where the disease has taken a huge toll, the coronavirus arrived in Australia and New Zealand in mid-summer. Most of the inhabitants of these two countries are descendants of pale-skinned British settlers (and convicts in the case of Australia). Yet at the same time the death rate in Great Britain, the homeland of their ancestors, is over 600 per million.
This suggests that sunshine, and, specifically, the sunshine vitamin, are responsible for the difference. If you look at the death rates throughout the world, it becomes apparent that countries in the southern hemisphere fared much better than countries north of the equator.
Actually, the division between countries with high death rates and low death rates is about the 37th parallel north. According to Wikipedia, the 37th parallel is the dividing line between greater than average and less than average sun exposure.
So it appears that people living south of the equator, and south of the 37th parallel north, experienced, in general, higher levels of sun exposure and lower death rates from the coronavirus than those in the northern hemisphere north of the of the 37th parallel.
This explains the very low death rates observed in Africa. Many experts have forecast that the coronavirus would take a heavy toll in Africa because of poor healthcare infrastructure in much of the continent. Yet this has not happened. For example, death rates in Ghana, Nigeria, Kenya, Ivory Coast, Togo, South Sudan, Niger and Burkina Faso are between 2 and 3 per million.
Virtually all of the continent is south of the 37th parallel north and sub-Saharan Africa is close to the Equator. It could be argued that the low death rate is an artifact of poor record keeping, but reasonably good data about another virus, Ebola, reached world attention, so high death rates from coronavirus would likely be evident.
The same is true in the Far East. Indonesia, Malaysia, Singapore and Sri Lanka are near the equator and have coronavirus death rates per million of 8, 4, 4, and 0.5. But this pattern breaks down when one looks at that most equatorial of nations, Ecuador.
Here the reported coronavirus death rate is about 223 per million. Other major countries of the South American continent, Brazil, Peru, Chile and Bolivia, have per million death rates of 208, 208, 176, and 54, which is quite a contrast to those seen in Africa and Southeast Asia. The disparity may arise from a greater susceptibility to the coronavirus among people with indigenous ancestry.
Support for this idea comes from the death rates in Argentina and Uruguay, which are 19 and 7, per million, respectively. Unlike the rest of South America, the populations of these two countries are very largely of European ancestry, mostly Spanish and Italian. Remember that while it was summer in Argentina and Uruguay, at the same time it was winter in Spain and Italy, where COVID-19 death tolls per million were 580 and 571, respectively.
This analysis supports the idea that the virulence of the coronavirus, as measured by death rate, varies inversely with sun exposure. Where the coronavirus struck during the summertime, in the southern hemisphere, death rates were very low, in very marked contrast to countries in the higher latitudes of the Northern Hemisphere, where the coronavirus struck in mid-winter. The cause proposed to explain this disparity is Vitamin D levels in the respective populations. How does that work?
Vitamin D3 is created in the skin by the ultraviolet light in sunlight. Before the advent of dietary supplements, sunlight was the only significant source of Vitamin D3. Fatty fish is a natural dietary source. Vitamin D3 is transformed inside the body to calcidiol, 25(OH)D3, which is not a vitamin, but a hormone.
Calcidiol has a half-life in the body of 2 to 3 weeks, so serum levels decline if they are not continually replenished by sun exposure or dietary supplements. Winters in the higher latitudes diminish sun exposure due to shorter days, lower sun angle (if the sun is lower than 45 degrees in the sky, little UV light makes it through the atmosphere), and the need to bundle up or stay indoors in cold weather.
About 15 years ago it was discovered that Vitamin D is critical to the proper function of the innate immune system. Broadly, there are two kinds of immunity – innate and acquired. The body acquires immunity when it creates antibodies in response to infection by a specific pathogen. This is the principal behind vaccines – to trigger the creation of antibodies.
However, the body also has an innate immune system that responds to the wide range of pathogens to which it is exposed every day. Recently it has been demonstrated that the innate immune system is the body’s principal defense against another viral disease – influenza. The annual wintertime outbreaks of influenza are triggered by declining levels of serum vitamin D in the host population. That is why influenza doesn’t occur in the summer and is very uncommon in the tropics.
For in-depth discussion of innate immunity, Vitamin D3 and influenza, read the paper in Virology Journal titled “On the Epidemiology of Influenza” by John Cannell, et. al., and his earlier paper “Epidemic Influenza and Vitamin D” published in the journal Epidemiology and Infection. Open access full text of both articles can be found on the internet on PubMed.
However, the COVID-19 coronavirus is not influenza, so the role of innate immunity and Vitamin D in the incidence and virulence of this disease must be established. Given the very recent emergence of COVID-19, it is understandable that not very much research on the role of Vitamin D has been published.
However, one key paper has come out, which has been summarized in the website Grassroothealth.net/blog/first-data-published-covid-19-severity-vitamin-d-levels/. The data are observational and the population of patients was 212, but the results are statistically significant. People with adequate levels of serum Vitamin D in their blood experienced mild bouts of COVID-19, while those with inadequate levels suffered ordinary, severe or critical cases. The chart in the article illustrates these data.
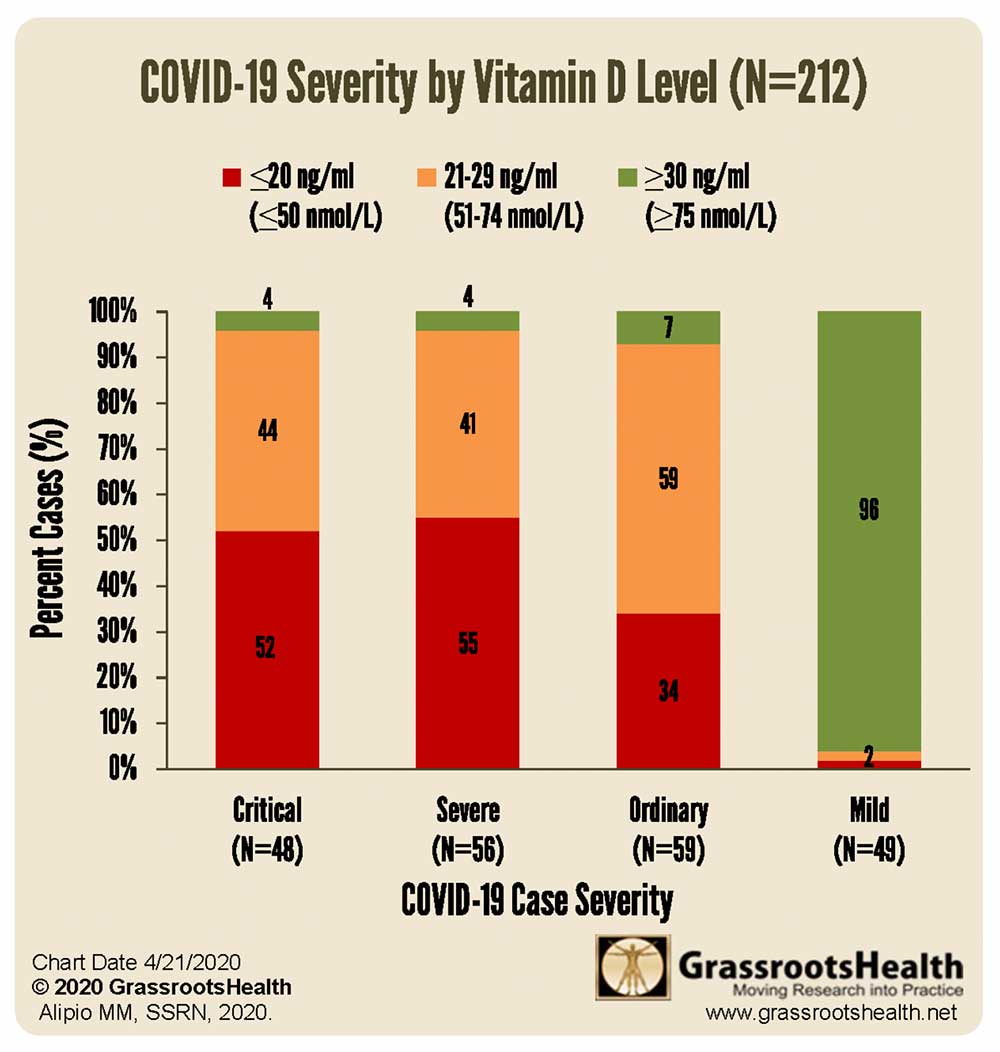
The results of this study are exactly consistent with the idea that sun exposure is inversely correlated with the virulence of COVID-19. When serum levels of Vitamin D are high, the disease is mild. When they are low, the disease is severe. Which then leads one to ask what are the specific effects of Vitamin D that reduce the severity of COVID-19 infection?
There are at least two. Severe cases can be complicated by what is called a “cytokine storm.” This is a severe over-reaction of the immune system that can be fatal. Vitamin D is known to prevent this condition (see the above-referenced articles by John Cannell). A second effect is related to the recent discovery that COVID-19 attacks blood vessels, in particular, the endothelium, which is the internal lining of vessels, causing widespread clotting1.
Research published in 2015 showed that Vitamin D3, in the form that is created in the skin by UV light or taken as a dietary supplement, has a direct, protective effect on the endothelium 2 Because Vitamin D3 lasts in the body only a day or so before it is processed into calcidiol, one needs a daily dose of sunshine or supplement to maintain the protective effect on blood vessels. It should be underscored that sunscreen blocks UV rays from reaching the skin and therefore diminishes the formation of Vitamin D. The skin pigment melanin is a natural sun screen and has a similar effect.
What does this mean for people who want to protect themselves from the malign effects of COVID-19? Vitamin D3 is not some untested off-label prescription drug or sketchy supplement: it is an essential hormone naturally produced in the human body by sunlight on the skin.
With enough sun, one’s body makes all that is necessary to counteract the virus. But modern lifestyles can make it impossible for many people to get sufficient daily sun exposure in the summer, and during Minnesota winters it is physically impossible because the sun is too low in the sky, not to mention that it is too cold to take off your clothes.
Therefore, one needs a program of supplementation with Vitamin D3, which is readily available over the counter. The question, of course, is how much. Grassrootshealth has devoted considerable study to finding the answer, a good discussion of which can be found here 3 The coronavirus statistics I used are from the site Worldometers 4
https://drmalcolmkendrick.org/